Clinical Handbook of Mindfulness (109 page)
Read Clinical Handbook of Mindfulness Online
Authors: Fabrizio Didonna,Jon Kabat-Zinn
Tags: #Science, #Physics, #Crystallography, #Chemistry, #Inorganic
just kind of didn’t matter. It didn’t matter where I got it from.
Sylvia described increased
acceptance
of what is occurring in the present
moment.
So, I learned how to be in the present and I use that a lot on a daily basis –
when I’m stressed out, you know even in traffic. You say, “I’m here now. This
is where I’m going to be. I’ll worry about the grocery store later.” I just accept
things a lot easier now than I did before.
Issues around
spirituality
, encompassing feelings of hope, peace, and
understanding, surfaced and resonated strongly with Sylvia despite that the
focus of the MBSR program is secular and does not specifically address
spirituality.
After the [full-day meditation] retreat I said that I was at such peace and it was
so spiritual
. . .
The increased feelings of spirituality and peace expressed by Sylvia had
particular implications related to her own experience of cancer.
I’m at peace. I understand it [the cancer] a lot better. I understand it. And if it
recurs, I think I’m prepared for that. [
. . .
] I know things happened for a reason,
always. Always.”
This comment is congruent with the definition of spirituality as an ability
to see the divinity, or greater organization in life, and to use this understand-
ing to deal with life challenges.
Significant increases in
PTG
were also evident in Sylvia’s interview. She
described experiencing positive changes related to the cancer experience
after participation in the program, and linked specific skill acquisition in deal-
ing with the cancer experience to her participation in the MBSR course.
I always knew that there was something that I had to learn from this and I
never knew what it was – I never knew. And I think now what I’ve learned
(and probably from the course) is, what I’ve learned is to appreciate things, to
take time for things, which I think before I was always so busy and always so
controlling, and you know, quite bossy. I realized that you can’t do anything
about the cancer but you can do something about how you feel about it and
how you react to it.
It is clear from this interview that many of the themes of the program
resonated with Sylvia’s experience of learning MBSR, particularly around
Chapter 20 Mindfulness-Based Interventions in Oncology
395
issues of feeling a need to know and have some certainty about why can-
cer occurred, and whether it was coming back. This inherent uncertainty
in the illness experience is often one of the most difficult issues for cancer
survivors to live with. Sylvia’s comments provide some insight into how the
program can help patients find peace even within this vast inability to know
the future with any degree of certainty. Somehow through the practice she
learned to tolerate uncertainty and uncontrollability much better than before
her cancer experience.
Sylvia’s responses during this qualitative interview represent only one
patient’s perception of the effects of MBSR on positive and negative out-
comes, but do resonate well with what other patients have articulated. The
interviews in general reveal a broad range of improvements related to a
greater appreciation for life and improved coping self-efficacy. Encourage-
ment of the adoption of attitudes such as acceptance and letting go appear
to have contributed to patients’ increased feelings of spirituality and PTG,
and decreased stress and mood disturbance. Based on qualitative analyses,
there appears to be a strong link between mindfulness practice and a health-
ier view of the cancer experience and its impact on daily functioning.
Summary and Conclusions
Distress and other negative reactions to a cancer diagnosis and all that it
entails are common and expected experiences for cancer patients and their
families. Fears of premature death and of the pain and indignities of can-
cer treatment are natural and well founded in many cases. Despite the hur-
dles such experiences present, patients are often able not only to adjust to
such a massive life stress, but even to thrive and grow as a result. We have
reviewed the rational suggesting MBSR may be helpful for cancer patients
and families, and provided an overview of the clinical research detailing its
efficacy for alleviating a wide range of negative outcomes including stress
symptoms, anxiety, anger, fear, sleep disturbance and depression. We have
also shown evidence of enhancement in overall quality of life, improved
ability to find benefit in the situation and grow through trauma, includ-
ing enhancement of a sense of spirituality and meaning and purpose in
life, as well as enhanced ability to tolerate uncertainty. In addition to these
psychological benefits, patients often show improved biological regulation
of a variety of circadian systems that are essential to promote health and
homeostasis, such as cytokine expression, cortisol secretion, and blood pres-
sure. We have attempted to integrate methods of inquiry including both
qualitative and quantitative approaches in the hopes of better understand-
ing not only the outcomes of MBSR in people living with cancer, but also
the potential mechanisms that may help to explain how and why MBSR
is effective in this group. Future research efforts of our group and others
should help to lend further understanding not only to the full range of
effects of MBSR, but also some insight into these intriguing questions of
how and why.
Acknowledgements:
Dr. Linda E. Carlson holds the Enbridge Endowed
Research Chair in Psychosocial Oncology, co-funded by Enbridge Inc., the
396
L.E. Carlson et al.
Canadian Cancer Society, and the Alberta Cancer Foundation. Laura E. Labella
is funded by an Alberta Heritage Foundation Medical Research PhD Schol-
arship and a Social Sciences and Humanities Research Counsel of Canada
PhD Fellowship, and Sheila Garland is funded by the Social Sciences and
Humanities Research Counsel of Canada PhD Fellowship. The research
described in this chapter has been funded by the Canadian Institutes of
Health Research, National Cancer Institute of Canada, Canadian Breast Can-
cer Research Alliance, and Calgary Health Region through grants awarded to
Dr. Linda E. Carlson. None of this work would be possible without the co-
operation and dedication of the patients who have given generously of their
time to participate in our research programs – heartfelt thanks are extended
to them all.
Appendix: Description of Specific Didactic Learning and
Experiential Exercises
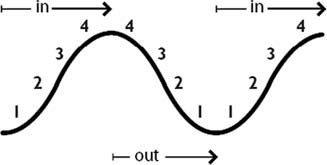
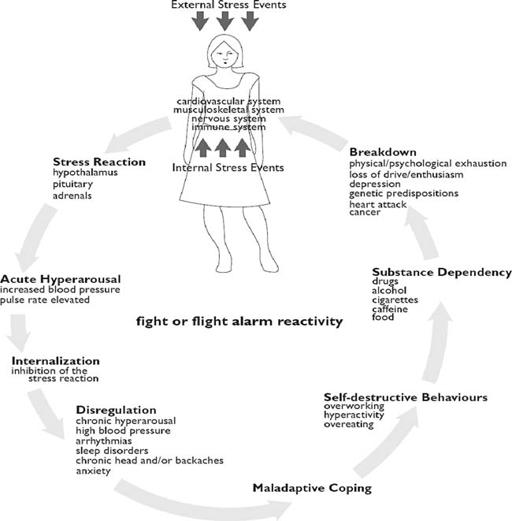
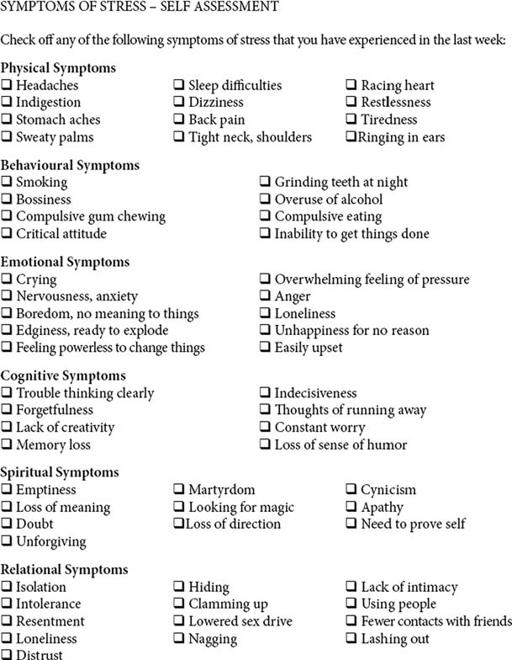
Following group discussion and problem solving about home practice, the
didactic components of Week 3 (“Mind-body Wisdom and Healing”) and
Figure. 20.1.
The stress reaction.
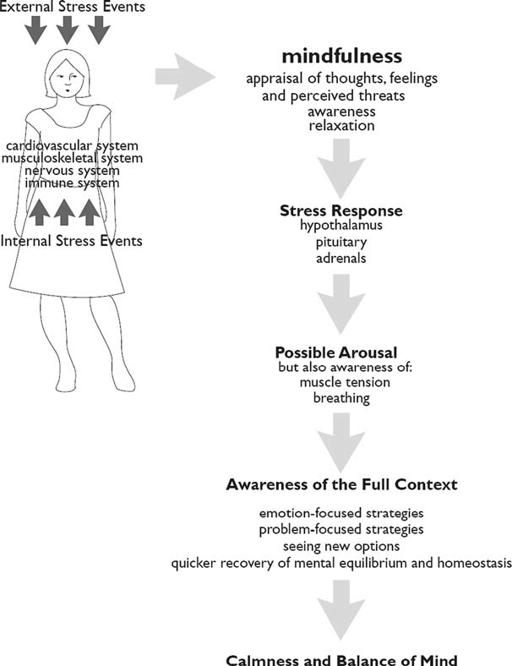
Chapter 20 Mindfulness-Based Interventions in Oncology
397
Week 4 (“Balance in the Autonomic Nervous System”) in our MBSR pro-
gram include a description of the automatic physical, emotional and behav-
ioral reaction to stress, compared with the response when we choose
to attend mindfully to our experience. Short and long-term emotional,
cognitive, behavioral, and physiological aspects of these two different
responses are illustrated and discussed (Figures
20.1
and
20.2;
adapted from
Kabat-Zinn, 1990).
In addition, participants complete a self-assessment checklist of symptoms of stress, in order to develop awareness of the
ways in which stress may influence emotions, sensations, and behaviors
(Figure
20.3).
In Weeks 3 and 4, following didactic instruction, participants are guided
through a series of experiential exercises involving bringing awareness to
Figure. 20.2.
The stress response.
398
L.E. Carlson et al.
Figure. 20.3.
Symptoms of stress self-assessment.
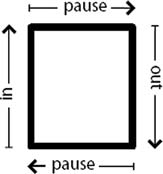
the breath. These are taught in conjunction with the basic sitting medita-
tion and yoga postures that occur during each weekly class. These exercises
are referred to as “mini” mindfulness exercises. “Minis” are focused breathing
techniques that are practiced to help reduce anxiety and tension in any place,
at any time, and can be engaged in without others taking notice. For example,
“minis” can be performed when stuck in traffic, when feeling overwhelmed,
when waiting in the doctor’s office, waiting in line or when experiencing
pain. Participants are guided through the experience of mindful slow, deep
diaphragmatic breathing then use the various techniques to focus breath pat-
terns and awareness (Figures
20.4–20.8).