Clinical Handbook of Mindfulness (58 page)
Read Clinical Handbook of Mindfulness Online
Authors: Fabrizio Didonna,Jon Kabat-Zinn
Tags: #Science, #Physics, #Crystallography, #Chemistry, #Inorganic
follow-up.
More than a therapeutic technique, it might be more appropriate to say
that PEV is a mindful mental style or attitude. It is an alternative way for OCD
patients to relate to themselves and their experience, helping them see that
certainty is unnecessary because the information that they already possess is
sufficient.
OCD Problem Formulation and Mindfulness
As has been pointed out by
Teasdale et al. (2003),
when a mindfulness-based intervention is provided for individuals with specific disorders, it is particularly important to share with patients, both in individual and group settings,
a clear problem formulation explaining the potential role of the mindful state
in order to prevent the maintaining mechanisms of the disorder. Mindfulness
training is effective when it is linked to coherent alternative views of patients’
problems, views that are shared with patients and reinforced through the
mindfulness practices
(Teasdale et al., 2003).
Chapter 11 Mindfulness and Obsessive-Compulsive Disorder
207
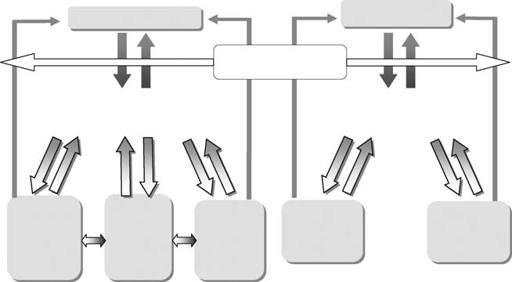
Anxiety disorders are activated and maintained by dysfunctional metacog-
nitions about normal and innocuous mental events. Following the standard
cognitive conceptualizations of psychological disorders, the clinical rele-
vance of mindfulness for several diseases, and for OCD too, might lie in its
intervening at a radical and hierarchically superordinate level, in particular,
at a point between inner and outer activating stimuli and the metacognitive
processes and maintaining mechanisms conducive to psychological distress
(Figure 11.3). Mindfulness, which is a
being mode
(see Chapter 1), can be
cultivated to prevent or deactivate the metacognitive processes which lead
patients into the vicious, self-perpetuating cycles of obsessions and the asso-
ciated counterproductive behaviors.
(Didonna, 2006, 2008).
If we compare OCD with a related diagnosis such as panic disorder, we
can observe that in both disorders the problem stems from how some nor-
mal experiences are perceived (Figure 11.3). Looking at a standard cognitive
model of these problems, in the case of the obsessive-compulsive syndrome,
the trigger is normally an intrusive cognition, while in panic disorder, in the
trigger is one or more normal physical sensations. Subsequently, the patient
starts to interpret these normal experiences as dangerous (metacognition),
which in the case of OCD may involve a pervasive idea of responsibility
for harm or damage, while in panic disorder it will involve a thought of
imminent catastrophe. These two meta-evaluations then activate the main-
tenance mechanisms of the two disorders: “Doing mode” (neutralization,
rituals, seeking reassurance, rumination) and cognitive biases (perceptive
self-invalidation, attentional biases, thought-action fusion, non-acceptance
bias) on the one hand and
safety seeking behavior
on the other (avoid-
ance, flight, etc.), but also emotional states, anxiety, guilt, shame, disgust,
depression in OCD and anxiety in Panic, which will reinforce the initial
metacognitions that maintain the disorder. Compulsions, neutralizations,
and safety behaviors are acts that are performed in an attempt to reduce
Obsessive-Compulsive
Panic
Disorder
normal sensations
normal intrusive cognitions
State of Mindfulness
FACTORS
(“bein
ng mode””)
META-EVALUATION
Misinterpretation of intrusions
META-EVALUATION
based on hyperactivation of OCD belief
misinterpretation of sensations
ACTIVATING
domains (e.g. inflated responsibility)
In terms of catastrophic belief
Perceptive self-
“Doing mode”
“Doing mode”
invalidation,
Emotional
neutralization,
Safety-seeking
attentional
states
Anxiety
rituals,
Behaviour
biases,
reassurance,
(anxiety, guilt,
(avoidance and
thought-action
rumination
fusion, non-
shame, disgust
flight)
acceptance
depression)
MAINTENANCE FACTORS
Figure. 11.3.
A cognitive formulation of the role and effects of mindfulness state and
practice with respect to the activating and maintenance factors in OCD and panic
disorder.
208
Fabrizio Didonna
the perceived threat and the anxiety and distress caused by the metacog-
nitions, but the relief is only temporary: indeed, these behaviors increase,
rather than reduce, the anxiety. These reactions maintain the problem and
prevent habituation to the anxiety and disconfirmation of the patient’s fears
(Didonna,
Salkovskis, 1996,
2006, 2008).
The activation of a mindful state (a “being mode”) intervenes at an early
stage in the activation of the symptoms of these disorders, allowing the
patient to take a different attitude toward “normal” internal initial experi-
ences (thoughts, sensations) from the moment he/she becomes aware of
them, by means of an accepting, self-validating, and non-judgmental attitude.
Such an attitude, cultivated through mindfulness practice, prevents the acti-
vation of those meta-evaluational processes that would otherwise give rise to
the anxious syndrome (Figure 11.3).
Mindfulness training can help OCD patients inhibit secondary elaborative
processing of the thoughts, feelings, and sensations that arise in the stream
of consciousness and may cause improvements in cognitive inhibition,
particularly at the level of stimulus selection
(Bishop et al., 2004).
This effect can be objectively evaluated using specific tests that involve the inhibition
of semantic processing (e.g., emotional Stroop; Williams, Mathews, &
MacLeod,
1996).
Integrating CBT and Mindfulness
Always do what you are afraid to do!
Ralph Waldo Emerson
Unlike standard CBT, in mindfulness-based interventions the main goal is
not to change the content of the patient’s system of cognitions but rather to
change his or her way of relating to it. During mindfulness training, patients
are helped to shift from a focus on the past and on the future (conditioned
by memories and rumination) to a focus on the present moment, develop-
ing a process of
decentering
and
disidentification
from personal experi-
ence
(Segal et al., 2002).
Mindfulness-based treatments focus on altering the
impact
of and
response
to thoughts, emotions and sensations. It can thus be
particularly effective for a disorder like OCD in which intolerance of negative
inner experience and consequent behavioral avoidance play a central role.
Nevertheless, carrying out mindfulness interventions with obsessive
patients is not always easy, especially in the case of patients with severe or
chronic suffering. Such patients normally have rigid schemata and attitudes
toward their inner experience. One solution to this challenge also suggested
by other authors
(Schwartz & Beyette, 1997;
Hannan & Tolin, 2005;
Wilhelm
& Steketee,
2007;
Fairfax, 2008),
and that is adopted at the Mood and Anxiety Disorders Unit in Vicenza, is to integrate CBT with a mindfulness-based
intervention. This integration may be usefully provided in three phases, sum-
marized as follows:
(1)
Problem formulation
. This may be done during some preliminary ses-
sions in which therapist and patient reach a clear and shared conceptu-
alization of the activating and maintaining factors of OCD
(Salkovskis,
1985)
and the possible role and effects of mindfulness in this pro-
cess (see Figure 11.3). This allows the patient to understand how
Chapter 11 Mindfulness and Obsessive-Compulsive Disorder
209
his/her problem works and how mindfulness training might challenge
the dysfunctional mechanisms highlighted by the problem formulation.
Mindfulness may ameliorate OCD deficits, change the modes and the
maintaining factors of the disorder, help the patient modify how he/she
relates to the entire experience (inner and outer), and develop a new
way of being
.
(2)
Training
patients in Mindfulness skills. For this purpose it is useful to
provide patients with an already established and structured mindfulness-
based group, such as MBCT or MBSR, that has been adapted for OCD
patients. In this group, the importance and effects of exposure are high-
lighted, psychoeducational materials provided, and an explanation given
of how obsessive individuals relate to their thoughts, emotions and per-
ceptions. The mechanisms by which mindfulness can alter dysfunctional
OCD attitudes are also illustrated.
(3)
Integrating Exposure and Response Prevention (ERP) techniques and
mindfulness
using
mindful exposure
. Unlike classical ERP techniques,
in this form of exposure, the patient is continuously invited to stay
directly in touch with his/her private experience, carefully noticing,
moment by moment, the real cognitive, sensory and emotional expe-
rience which arises during exposure, without judgement, evaluation or
reaction to it, preventing on purpose any metacognitive processes on
the real experience, or seeing any metacognitions as simply thoughts,
and passing through it.
Anecdotal clinical experience with dozens of patients with OCD has sug-
gested that sessions (in individual or group setting) should follow the follow-
ing format (see Figure 11.4):
Practice of mindfulness
(Mindfulness of breath/body)
Exposure (in vivo or imagery) to anxiogenic stimuli
“Breath as an anchor”
Awareness of thoughts, sensations, feelings and emotions
and actively observing and describing private experience without judgment
Using allowing, ‘letting be’, acceptance attitudes towards
thoughts, sensations and emotional states
Using decentering, defusion and disidentification strategies;
‘thoughts as impermanent mental facts’
Using metaphors (e.g. “thoughts like clouds in the sky”)
Response Prevention – avoiding any overt and covert reaction to private
experience
(neutralizations, rituals, reassurance seeking)
Short mindfulness exercise (e.g. Breathing space)
Figure. 11.4.
Example of an integrated model of exposure and response prevention
procedure and mindfulness-based intervention.
210
Fabrizio Didonna
(A) The session should start by inviting the patient to practice a mindfulness
exercise which allows him/her to enter into a stable, balanced and wake-
ful state of mind (e.g., sitting meditation, body scan – see Appendix A),
fully opening attentive and sensory processes.
(B) The patient should be exposed (in vivo or imaginal exposure) to anxiety-
provoking or distressing situations or triggers. In each moment of this
phase, it is important to invite the patient to bring attention to an
“attentional anchor” or “mindfulness center” (e.g., the body or a sensory
input such as breathing) in order to be centered in the present moment
(“breathing as an anchor”) observing whatever happens in the inner and
outer experience.
(C) The patient should pay attention and bring awareness to any thoughts,
sensations, feelings and emotions that may arise and actively observe and
describe this private experience over and over again without judgment.
For example, anxiety may be described by the patient as an array of
innocuous physical sensations and thoughts whose increase cannot lead
to any dangerous consequences.
(D) The attitudes to be used are allowing, “letting be,” and acceptance
attitudes (learned at the mindfulness training) toward thoughts, sen-
sations and emotional states. Decentering, defusion and disidentifica-
tion strategies are used and for this purpose it might be useful to use