i bc27f85be50b71b1 (145 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown







BURNS AND WOUNDS
469
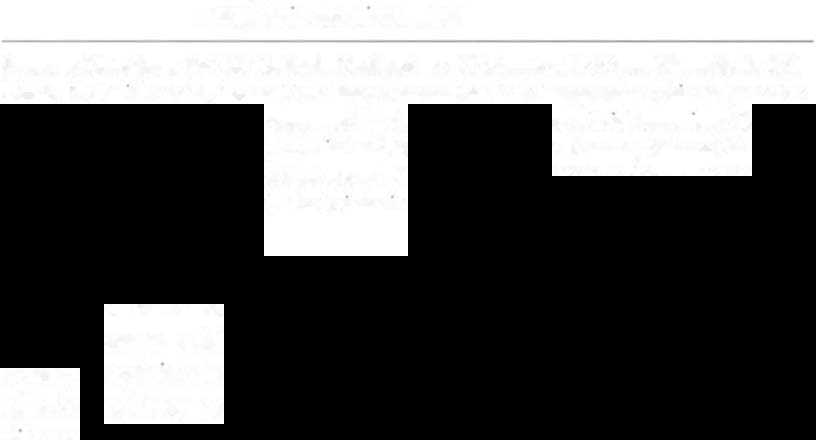
Table 7-11. Clinical Indicators of Vascular Insufficiency Wounds
and Diabctic Ulcers
Wound Etiology
Clinical Indicators
Arterial insuffi·
Intermirtent claudication
ciency
Extreme pain, decreased with rest and increased with
clevmion
Decreased or absent pedal pulses
Decreased temperaturc of the distal limb
Distinct, well-defined wound edges
Deep wound bed
Cyanosis
Venous
Localized limb pain, decreased with elevation and
Insufficiency
increased with srandmg
Pam with deep pressure or palpation
Pedal pulses present
Increased temperature around the wound
Indistinct, Irregular edges
Edema Mound the wound
Shallow wound bed
Suhsranrial drainage
Diabetic ulcer
Painless ulcer; however, general lower-limb pain is
present
Absent pedal pulses
Decreased temperature in the distal limb
Deep wound bed frequently located at pressure points
(e.g., metatarsal heads)
Shin}- skill on dlsral limb
Sources: D.lt.1
from JM �1cC:ulloch. r\'alu:lrion of P:lticnrs with Opcn Wounds. In LC
Kloth. KH M111er (cds), Wound Ilc:lhnlt: Alternatives in Management. Ph1ladelphia: FA
Da\·is, 1995; RG Sihbald. An approach to leg and foot ulcers: a bnef overv1ew. Ostomy
Wound MJnage 1998;44:29; RG �Ibbald. Venou!t leg ulcers. Osromy Wound Manage
1998;44:53; P Lamg. DI;Ibcrif.: foot ukcrs. AmJ Surg 1994;167(IA):31; and ML Levin,
LW O'Ncill, JII Bowker (cd�). Thc D1abetlc Foot (5th cd). St. loUIS: Mosby, 1993.
superficial veins in the subcutaneous tissue and [he overlying skin,
which causes widening of the capillary pores.J4.JS Clinically, this
would result In the first sign of venous disease, which is the presence
of a dilated long saphenous vein on the medial aspect of the calf. This
dIlation allows the escape of large macromolecules, including fibrinogen, into the interstitial space. This results in the development of edema toward the end of the day because of the pooling of fluid in the


470
AClITE CARE HANDBOOK FOR PHYSICAL TIIE.RAI'ISTS
dermis. In long-standing venous disease, fibrin accumulates in the dermis, creating a fibrin cuff that presents as hard, non pitting edema, and the surface skin is rigid and fixed. The theory states that this
fibrin cuff forms a mechanical barrier to the transfer of oxygen and
other nutrients, which progressively leads to cellular dysfunction, cell
death and skin ulceration.H."
Another hypothesis is called the white blood cell-trappil1g hypothesis. This theory states that transient elevations in venous pressures decrease capillary blood flow, resulting in trapping of white blood cells
at the capillary level, which in turn plugs capillary loops, resulting in
areas of localized ischemia." These white blood cells may also become
activated at this level, causing the release of various proteolytic
enzymes, superoxide free radicals, and chemotactic substances, which