Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine
Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (5 page)
• Radionuclide: ≥1 lg or ≥2 mod. reversible defects, transient LV cavity dilation, ↑ lung uptake
Myocardial viability (
Circ
2008;117:103;
Eur Heart J
2011;31:2984 & 2011;32:810)
• Goal: identify hibernating myocardium that could regain fxn after revascularization • Options:
MRI
(Se ~95%, Sp ~85%),
PET
(Se ~90%, Sp ~65%),
dobutamine stress
echo
(Se ~80%, Sp ~80%);
SPECT/rest-redistribution
(Se ~85%, Sp ~70%)
In Pts w/ LV dysfxn, viabil. doesn’t predict ↑ CABG benefit vs. med Rx (
NEJM
2011;364:1617)
CT & MR coronary angio (
NEJM
2008;369:2324;
Circ
2010;121:2509;
Lancet
2012;379:453)
• Image quality best at slower & regular HR (? give bB if possible, goal HR 55–60) • Calcium generates artifact for CT angiography • MRI: angiography, perfusion, LV fxn, enhancement (early = microvasc obstr; late = MI)
Coronary artery calcium score
(CACS;
Circ
2010;122:e584;
NEJM
2012;366:294;
JAMA
2012;308:788)
• Quantifies extent of calcium; thus
estimates
plaque burden (but
not
% coronary stenosis) • ? Risk strat. (<100 = low; >300 = high) in asx Pts w/ intermed risk (10–20% 10-y risk) • ? Value as screening test to r/o CAD in sx Pt (CACS <100 → 3% probability of signif CAD; but interpretation affected by age, gender)
CORONARY ANGIOGRAPHY AND REVASCULARIZATION
Indications for coronary angiography in stable CAD or asx Pts
• CCS class III–IV angina despite medical Rx or angina + systolic dysfxn • High-risk stress test findings (see prior topic) • Uncertain dx after noninvasive testing (& compelling need to determine dx), occupational need for definitive dx (eg, pilot) or inability to undergo noninvasive testing • Systolic dysfxn with unexplained cause • Survivor of SCD, polymorphic VT, sustained monomorphic VT
• Suspected spasm or nonatherosclerotic cause of ischemia (eg, anomalous coronary)
Precath checklist
• Document peripheral arterial exam (radial, femoral, DP, PT pulses; bruits); NPO >6 h • ✓ CBC, PT, & Cr; give IVF (± bicarb, ± acetylcysteine; see “CIAKI”); blood bank sample • ASA 325 mg × 1; consider clopi 600 mg ≥2–6 h before PCI or, if ACS, ticagrelor pre-or peri-PCI or prasugrel peri-PCI; cangrelor (IV P2Y
12
inhib) ↓ peri-PCI ischemic events vs. clopi w/o preload (
NEJM
2013;368:1303); consider statin preRx (
Circ
2011;123:1622)
Coronary revascularization in stable CAD (
Circ
2011;124:e574)
• Optimal med Rx (
OMT
) should be initial focus if stable, w/o critical anatomy, & w/o ↓ EF
•
PCI
: ↓ angina more quickly c/w OMT; does
not
↓ D/MI (
NEJM
2007;356:1503); in Pts w/ ≥1 stenosis w/ FFR ≤0.8 (see below), ↓ urg revasc c/w OMT (
NEJM
2012;367:991); may be noninferior to CABG in unprotected left main dis. (
NEJM
2011;364:1718) •
CABG
: in older studies, ↓ mort. c/w OMT if 3VD, LM, 2VD w/ critical prox LAD, esp. if ↓ EF; more recently, if EF <35% ↓ CV death vs. OMT (
NEJM
2011;364:1607) insufficient evidence to support routine viability assessment (
NEJM
2011;364:1617) in diabetics w/ ≥2VD, ↓ D/MI, but ↑ stroke c/w PCI (
NEJM
2012;367:2375) • If revasc deemed necessary,
PCI
if limited # of discrete lesions, nl EF, no DM, poor operative candidate;
CABG
if extensive or diffuse disease, ↓ EF, DM or valvular disease; if 3VD/LM: CABG ↓ D/MI & revasc but trend toward ↑ stroke c/w PCI (
Lancet
2013;381:629); SYNTAX score II helps identify Pts who benefit most from CABG (
Lancet
2013;381:639)
PCI
•
Balloon angioplasty (POBA)
: effective, but c/b dissection & elastic recoil & neointimal hyperplasia → restenosis; now reserved for small lesions & ? some SVG lesions •
Bare metal stents (BMS)
: ↓ elastic recoil → 33–50% ↓ restenosis & repeat revasc (to ~10% by 1 y) c/w POBA; requires ASA lifelong & P2Y
12
inhib × ≥4 wk •
Drug-eluting stents (DES)
: ↓ neointimal hyperplasia → ~75% ↓ restenosis, ~50% ↓ repeat revasc (to <5% by 1 y), no ↑ D/MI c/w BMS (
NEJM
2013;368:254); next generation DES may ↓ repeat revasc & stent thrombosis; require P2Y
12
inhib ≥1 y (
Circ
2007;115:813) • Radial access ↓ vasc. complic. vs. femoral, but no ∆ D/MI/CVA (
Lancet
2011;377:1409) • Fractional flow reserve [FFR; ratio of max flow (induced by IV or IC adenosine) distal vs. proximal to a stenosis] guided PCI (<0.8) → ↓ # stents & ↓ D/MI/revasc (
NEJM
2009;360:213)
Post-PCI complications
• Postprocedure ✓ vascular access site, distal pulses, ECG, CBC, Cr •
Bleeding
hematoma/overt bleeding:
manual compression
, reverse/stop anticoag
retroperitoneal bleed:
may p/w ↓ Hct ± back pain; ↑ HR & ↓ BP late; Dx w/ abd/pelvic CT (I
–
); Rx: reverse/stop anticoag (d/w interventionalist), IVF/PRBC/plts as required
if bleeding uncontrolled, consult performing interventionalist or surgery
•
Vascular damage
(~1% of dx angio, ~5% of PCI;
Circ
2007;115:2666)
pseudoaneurysm: triad of pain, expansile mass, systolic bruit; Dx: U/S; Rx (if pain or >2 cm): manual or U/S-directed compression, thrombin injection or surgical repair
AV fistula: continuous bruit; Dx: U/S; Rx: surgical repair
LE ischemia (emboli, dissection, clot): cool, mottled extremity, ↓ distal pulses; Dx: pulse volume recording (PVR), angio; Rx: percutaneous or surgical repair
•
Peri-PCI MI
: >5× ULN of Tn/CK-MB + either sx or ECG/angio Δs; Qw MI in <1%
•
Renal failure
: contrast-induced manifests w/in 24 h, peaks 3–5 d (see “CIAKI”) •
Cholesterol emboli syndrome
(typically in middle-aged & elderly and w/ Ao atheroma)
renal failure (late and progressive, eos in urine); mesenteric ischemia (abd pain, LGIB, pancreatitis); intact distal pulses but livedo pattern and toe necrosis
•
Stent thrombosis
: mins to yrs after PCI, typically p/w AMI. Due to mech prob. (stent underexpansion or unrecognized dissection, typically presents early) or
d/c of antiplt Rx
(esp. if d/c both ASA & P2Y
12
inhib;
JAMA
2005;293:2126). Risk of late stent thrombosis may be higher with DES than BMS (
JACC
2006;48:2584).
•
In-stent restenosis
: mos after PCI, typically p/w gradual ↑ angina (10% p/w ACS). Due to combination of elastic recoil and neointimal hyperplasia; ↓ w/ DES vs. BMS.
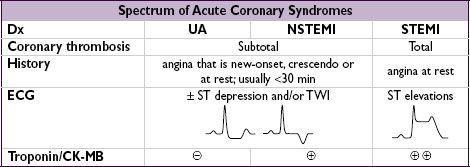
ACUTE CORONARY SYNDROMES
Ddx (causes of myocardial ischemia/infarction other than atherosclerotic plaque rupture)
• Nonatherosclerotic coronary artery disease
Spasm: Prinzmetal’s variant, cocaine-induced (6% of CP + cocaine use r/i for MI)
Dissection: spontaneous (vasculitis, CTD, pregnancy), aortic dissection with retrograde extension (usually involving RCA → IMI) or mechanical (catheter, surgery, trauma)
Embolism: endocarditis, prosthetic valve, mural thrombus, AF, myxoma; thrombosis
Vasculitis: Kawasaki syndrome, Takayasu arteritis, PAN, Churg-Strauss, SLE, RA
Congenital: anomalous origin from aorta or PA, myocardial bridge (intramural segment)
• Fixed CAD but ↑ myocardial O
2
demand (eg, ↑ HR, anemia, AS) → “demand” ischemia • Myocarditis; Takatsubo/stress CMP; toxic CMP; cardiac contusion
Clinical manifestations (
JAMA
2005;294:2623)
•
Typical angina
: retrosternal pressure/pain/tightness ± radiation to neck, jaw or arms
precip. by exertion, relieved by rest or NTG; in ACS, new-onset, crescendo or at rest
•
Associated symptoms
: dyspnea, diaphoresis, N/V, palpitations or lightheadedness • Many MIs (~20% in older series) are initially unrecognized b/c silent or atypical sx
Physical exam
• Signs of ischemia: S
4
, new MR murmur 2° pap. muscle dysfxn, paradoxical S
2
, diaphoresis • Signs of heart failure: ↑ JVP, crackles in lung fields,S
3
, HoTN, cool extremities • Signs of other areas of atherosclerotic disease: carotid or femoral bruits, ↓ distal pulses
Diagnostic studies
•
ECG
: ST ↓/↑, TWI, new LBBB, hyperacute Tw. Qw/PRWP may suggest prior MI, ∴ CAD ✓ ECG w/in 10 min of presentation, with any Δ in sx and at 6–12 h; compare w/ baseline
dx of STEMI if old LBBB: ≥1 mm STE concordant w/ QRS (Se 73%, Sp 92%), STD ≥1 mm V
1
–V
3
(Se 25%, Sp 96%) or STE ≥5 mm discordant w/ QRS (Se 31%, Sp 92%)
Other books
Lafcadio Hearn's Japan by Hearn, Lafcadio; Richie, Donald;
El Amante by Marguerite Duras
A Colder Kind of Death by Gail Bowen
Betraying the Duke by Sophia Wilson
Privy to the Dead by Sheila Connolly
Dreams of a Hero by Charlie Cochrane
Undertow by Kingston, Callie
Thunder & Lightning: We're all leaves in a hurricane. (Gifted) by Roberts, Patrick
His Firm Hand by Shelly Douglas