The Brain in Love: 12 Lessons to Enhance Your Love Life (32 page)
Read The Brain in Love: 12 Lessons to Enhance Your Love Life Online
Authors: Daniel G. Amen
Tags: #Family & Relationships, #Health & Fitness, #Medical, #Psychology, #Love & Romance, #Human Sexuality, #Self-Help, #Brain, #Neuroscience, #Sexuality, #Sexual Instruction, #Sex (Psychology), #Psychosexual disorders, #Sex instruction, #Health aspects, #Sex (Psychology) - Health aspects, #Sex (Biology)
Treat Brain Problems Early
If you have learning, mood, behavior, or memory problems, get an evaluation. The brain is an organ just like your heart or kidneys. When there are signs of trouble, work on getting it fixed.
Use these strategies to have the best brain possible. A better brain improves everything else in your life, including your sex life.
Lesson #12: Caring for your brain increases your chances for great sex
.
 The Amen Clinic Brain
The Amen Clinic Brain
System Questionnaire
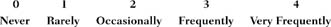
Please rate yourself on each of the symptoms listed below using the following scale. If possible, for the most complete picture, have another person who knows you well (such as a spouse, lover, or parent) rate you also.
PREFRONTAL CORTEX ISSUES (PFC)
1. Fails to give close attention to details or makes careless mistakes
2. Has trouble sustaining attention or trouble listening
3. Is poorly organized
4. Is easily distracted
5. Finds difficulty expressing empathy for others
6. Blurts out answers before questions have been completed, interrupts frequently
7. Is impulsive (saying or doing things without thinking first)
ANTERIOR CINGULATE GYRUS (ACG)
8. Excessive or senseless worrying
9. Upset when things do not go your way
10. Upset when things are out of place
11. Tendency to be oppositional or argumentative
12. Tendency toward compulsive behaviors
13. Intense dislike for change
14. Needing to have things done a certain way or you become very upset
DEEP LIMBIC SYSTEM (DLS)
15. Frequent feelings of sadness or moodiness
16. Negativity or irritability
17. Low energy
18. Decreased interest in things that are usually fun or pleasurable
19. Feelings of hopelessness, helplessness, worthlessness, or guilt
20. Crying spells
21. Chronic low self-esteem
BASAL GANGLIA (BG)
22. Frequent feelings of nervousness, anxiety, or panic
23. Symptoms of heightened muscle tension (headaches, sore muscles, hand tremor)
24. Tendency to predict the worst
25. Conflict avoidance
26. Excessive fear of being judged or scrutinized by others
27. Excessive motivation
28. Lack of confidence in abilities
TEMPORAL LOBES (TLs)
29. Short fuse or periods of extreme irritability
30. Frequent misinterpretation of comments as negative when they are not
31. Frequent periods of déjà vu (feelings of being somewhere you have never been)
32. Sensitivity or mild paranoia
33. History of a head injury or family history of violence or explosiveness
34. Dark thoughts, may involve suicidal or homicidal thoughts
35. Periods of forgetfulness or memory problems
ANSWER KEY
Prefrontal cortex (PFC) symptoms, 1–7: ____
Anterior cingulate gyrus (ACG) symptoms, 8–14: ____
Deep limbic system (DLS) symptoms, 15–21: ____
Basal ganglia (BG) symptoms, 22–28: ____
Temporal lobe (TL) symptoms, 29–35: ____
In each system, the following number of questions with the answer of 3 or 4 indicates that problems may be present in that area.
5 questions = Highly probable
3 questions = Probable
2 questions = May be possible
See Lesson Two for a description of the brain systems, problems, and treatments.
 Why SPECT?
Why SPECT?
What Brain-SPECT Imaging Can Tell Clinicians
and Patients That Cannot Be Obtained Elsewhere
If we agree that mental disorders and difficult behaviors may be related to functional problems in the brain, then a logical next step is clearly to consider physically evaluating the
brain itself
when faced with people who struggle with complex problems or who are unresponsive to our best diagnostic and treatment efforts. Why are psychiatrists the only physicians who rarely look at the organ they treat? It is time to change. Amen Clinics, Inc. (ACI) has provided leadership and understanding on the clinical use of brain imaging in psychiatry. Since 1991, ACI has built the world’s largest database of brain scans related to emotional, learning, and behavioral problems. The study we do is called brain-SPECT imaging. SPECT stands for Single Photon Emission Computed Tomography. It is a nuclear medicine procedure widely used in medicine to study heart, liver, thyroid, bone, and brain problems. Brain-SPECT imaging is a proven, reliable measure of cerebral blood flow. Because brain activity is directly related to blood flow, SPECT effectively shows us the patterns of activity in the brain.
1
SPECT allows physicians to look deep inside the brain to observe three things: areas of the brain that work well, areas of the brain that work too hard, and areas of the brain that do not work hard enough. ACI has performed more than 35,000 scans on patients from age 10 months to 101 years, and has also scanned many normal, “healthy brain” individuals as well.
The procedure guidelines of the Society of Nuclear Medicine lists the evaluation of suspected brain trauma, evaluation of patients with suspected dementia, presurgical location of seizures, and the detection and evaluation of cerebral vascular disease as common indications for brain SPECT.
2
The guidelines also say that many additional indications appear promising. At ACI, because of our experience, we have added the indications of evaluating violence, substance abuse, the subtypes of ADD, anxiety, and depression, and complex or resistant psychiatric problems for brain SPECT.
An important question for today’s mental health clinicians is “When and why would I order a SPECT study for my patients or get one for myself or a loved one?” My purpose in this section is to answer this question and to point out some of the benefits and caveats for using this powerful tool. A SPECT scan can provide distinct benefits to clinicians, and to the patient and his/her family. (There are also some things that should
not
be expected from a SPECT scan, listed later.)
Benefits for Physicians and Clinicians
A SPECT scan can show:
Areas of the brain implicated in specific problems, such as the prefrontal cortex with executive function and the medial temporal lobes with long-term memory storage.
Unexpected findings that may be contributing to the presenting problem(s), such as toxicity, potential areas of seizure activity, or past brain trauma.
Potential seizure activity, in many cases more accurately seen by SPECT than standard EEG, especially in the areas of the medial temporal lobe. There are more than forty-one studies with more than 1,300 patients on SPECT and epilepsy (see
www.amenclinic.com
for references).Targeted areas for treatment, such as overactive basal ganglia or anterior cingulate gyrus (seen on anxiety and OCD spectrum disorders) or an underactive temporal lobe (seen in seizure disorders and trauma).
Specific effects of medication on the brain to help guide us in adjusting dosages or augmenting treatment. Often patients report that SSRIs are helpful but also cause decreased motivation or memory problems, seen as decreased prefrontal or temporal lobe activity on SPECT.
Changes in brain function with treatment, improved or worsened. You can review many “before and after” scans at
www.amenclinic.com
.
The image occurs at the time of injection and outside the imaging camera, which gives SPECT several significant advantages. Most notably, we are able to sedate people after they have been injected so that they can lie still for the scan, often difficult for hyperactive or autistic children or demented adults (motion artifact ruins the scan in all of these imaging techniques).
A SPECT scan can provide explanations for refractory symptoms and help clinicians ask better and more targeted questions (e.g., about toxic exposure, brain injuries, anoxia, inflammation, or infections that patients may have denied or forgotten).
A SPECT scan can help us to avoid prescribing treatments that make the problem worse, such as unnecessarily stimulating an already overactive brain or calming an underactive one.
A SPECT scan can help to evaluate risk for dementia—the brain starts to change long before people show symptoms. There is usually a loss of 30 percent of hippocampal tissue before symptoms occur. Using autopsy data in fifty-four patients, Bonte reported that brain SPECT had a positive predictive value for Alzheimer’s disease of 92 percent.
3A SPECT scan can also help to differentiate between types of dementia. Early in the disease, Alzheimer’s disease, frontal temporal lobe dementia, Lewy body dementia, and multiinfarct dementia each have their own patterns. There are more than eighty-three studies with more than 4,500 patients on this subject (see
www.amenclinic.com
for references).A SPECT scan helps clinicians understand the rationale for using certain medications (such as anticonvulsants to stabilize temporal lobe function or to calm focal areas of marked hyperactivity, or stimulants to enhance decreased prefrontal perfusion, or SSRIs to calm basal ganglia and anterior cingulate hyperactivity).
A SPECT scan can identify specific areas of the brain affected by trauma, better target treatment, and help deal with insurance, legal, and rehabilitation issues. There are more than thirty-eight studies with more than 1,300 patients on brain trauma (see
www.amenclinic.com
for references).A SPECT scan can often identify factors contributing to relapse in recovering substance abusers, eating disordered, or sexual addicts. For example, the patient may have suffered an injury to the prefrontal cortex or temporal lobes or have overactivity in the anterior cingulate gyrus, basal ganglia, limbic system, or prefrontal cortex, each of which could indicate comorbid disorders requiring treatment.
A SPECT scan can often identify a specific cause or reason that contributes to recovering alcoholics, drug addicts, eating disordered, or sexual addicts relapse behavior in their recovery from an addictive process. For example, the patient may have suffered an injury in the prefrontal cortex or temporal lobes or have overactivity in anterior cingulate gyrus, basal ganglia, limbic system, or prefrontal cortex, each of which could contribute to the relapsing behaviors.
A SPECT scan is also useful to determine if further adjustment of medication is needed. Scans of patients on medication will reveal areas of the brain still overactive or underactive.