Vaccinated (17 page)
Authors: Paul A. Offit
In 1910, one year before Wright conducted his study, German researchers had found that there were two different types of pneumococci and that immunity to one didn't protect against infection from the other. By 1913, F. Spencer Lister, an English physician working in South Africa, had found four different types of pneumococci. More would follow. By the 1930s, researchers had identified thirty different types, and by the end of the Second World War, forty types. Today, researchers have identified at least ninety different types of pneumococci. Wright's attempts to protect South African gold miners failed because he didn't include enough different types of pneumococci in his vaccine. (Many of Almroth Wright's colleagues called him “Sir Almost Right.”) Researchers had to find a way to prevent a disease that could be caused by many immunologically distinct types of the same bacterium.
Where Wright failed, Robert Austrian, a researcher at the University of Pennsylvania, succeeded. Austrian, who grew up in a three-story, high-ceilinged brick row house on Baltimore's Doctors' Row, was the son of Charles Robert Austrian, physician-in-chief at Sinai Hospital and an associate professor at Johns Hopkins. “I was scared to death to go into medicine,” recalled Austrian. “My father was a hard act to follow.” A trim, well-spoken man of German Jewish ancestry, Austrian finished his internship and residency at Hopkins in 1945 and decided to pursue a career in infectious diseases. “I was told that if you wanted to learn classical bacteriology, go to Harvard or [the] Rockefeller [Institute]. But if you wanted to see the future of bacteriology, go to New York University.” At NYU Austrian met Colin MacLeod, the man who inspired his lifelong interest in pneumococcus. Austrian's interest in a pneumococcal vaccine would soon be interrupted by a medical product first developed in Germany.
Â
I
N
1908
A
V
IENNESE CHEMIST NAMED
P
AUL
G
ELMO SYNTHESIZED A
chemical thatâbecause it was bright redâproved very useful in the German dye industry. The dye also stained bacteria, which made them easier to see under a microscope. Twenty-five years later, a physician named Gerhard Domagk found that if he gave this dye to mice and rabbits, he could protect them against lethal doses of bacteria. Although the dye was effective in animals, Domagk hesitated to inject it into people. But in 1935, his young daughter became very ill with a streptococcal infection of her bloodstream, an often fatal disease. The crisis forced Domagk to act. In desperation, he gave her a dose of the dye, saving her life. The dye was called sulfanilamide, and it was the first antibiotic.
Austrian remembers the dawn of the antibiotic era: “Dr. Perrin Long [chairman of community medicine at Hopkins] was the first person to bring sulfa drugs back to the United States. The results of his treatment of several patients with streptococcal infections were so dramatic that some of his colleagues thought that he was lying. The possibilities seemed limitless.” Sulfa drugs appeared to be the magic bullet in the fight against bacterial infections. At Hopkins, Perrin Long was the keeper of the gate, the man in charge of a very limited supply of sulfa drugs. He took his charge seriously, as demonstrated by one memorable incident. A co-worker remembered a late-night phone call in 1936. “I answered it, and a woman's voice asked for Dr. Long. He took the phone, and I heard him say, âYou can't fool me this time! I know you're not Eleanor Roosevelt,' and he hung up. Within seconds the phone rang again. This time he said meekly, âYes, Mrs. Roosevelt, this is Dr. Long.' The next day the newspapers announced that the president's son was ill. Later, they reported that the boy had been cured by sulfanilamide, supplied by [Dr.] Long.”
By the early 1940s, researchers had found a method to mass-produce a different antibiotic, penicillin. Now, clinicians were confident that they could eliminate pneumococcal infections. “The drop in mortality was so dramatic,” recalls Austrian, “that most people began to feel that this illness was no longer a common or serious one. And not only that: they no longer felt that it was necessary to identify pneumococci; the recognition of the organism declined. The opinion in the 1940s and 1950s was widely held that pneumococcal pneumonia had largely disappeared because of these new so-called wonder drugs.” Austrian found, however, that while antibiotics saved lives, they didn't lessen the incidence of infection. “When I went from Hopkins to Kings County Hospital in Brooklyn, which was the third largest hospital in the United States, I was told that if I was really interested in pneumococcal pneumonia, I was probably in the wrong place because they saw so few cases every year.” Austrian set up a laboratory to determine how many people with pneumonia were infected with pneumococcus. “The place was a madhouse,” recalled Austrian. “There were four thousand beds. Beds were lined up in the corridors.” He found that about four hundred people every year were admitted to Kings County with pneumococcal pneumonia. Austrian's colleagues remained unconvinced, believing that his findings were unique to Brooklyn. “So we got a grant from the National Institutes of Health to look at the incidence of pneumococcal pneumonia throughout the United States because, as a wag once said, âBrooklyn is a city opposite the United States.' But it turned out there was just as much pneumococcal pneumonia coming into the city hospitals of Chicago, Los Angeles, and New Orleans as we had found in Brooklyn. It was very clear that the disease had not gone away. It was just a matter of seeing what you looked for.”
After ten years of collecting data, Austrian found another surprise. He examined the death rates in three groups of patients with severe pneumococcal infections: those who had been treated with antibiotics, those treated with antiserum (made from the serum of horses injected with pneumococci), or those left untreated. Although antibiotics and antiserum clearly saved lives, they didn't work on the most severe infections. “The death rates among those who died in the first five days were essentially the same,” said Austrian. “What this tells us is that if you are destined to die very early in illness, it won't make a difference what treatment we give you, because we don't understand even today [what's causing] early death. The only alternative then to protect those at high risk of early death is to prevent them from becoming ill.” Austrian was talking about a pneumococcal vaccine.
Â
B
ETWEEN
1900
AND
1945,
SCIENTISTS MADE SEVERAL IMPORTANT DISCOVERIES
about pneumococcus. They found that the bacterium was surrounded by a capsule made of a complex sugar called polysaccharide, that the polysaccharide could be stripped from the bacteria, that polysaccharide injected into mice protected them against infection, and that people injected with different polysaccharides from various strains of pneumococcus developed antibodies against each of the different types. Colin MacLeod, Austrian's mentor at NYU, made the first successful pneumococcal vaccine by taking four different types of pneumococci and stripping off their polysaccharide coats. During the Second World War, he injected either his vaccine or placebo into seventeen thousand military recruits and found that following an epidemic of pneumococcal pneumonia, his vaccine worked. E. R. Squibb made MacLeod's vaccine in the late 1940s, using six different types of pneumococcus. Nobody bought it. Convinced that penicillin had eradicated pneumococcus, doctors weren't interested in a pneumococcal vaccine. So Squibb stopped making it.
By the early 1970s Austrian, now a professor at the University of Pennsylvania, decided to resurrect Colin MacLeod's pneumococcal vaccine. “I was told [by university administrators] that I could do anything that I wanted as long as I paid for it,” he recalled. Austrian found that thirteen different types of pneumococcus accounted for a large percentage of the disease. So with support from the NIH, he made a vaccine containing polysaccharides from each of those types. Austrian and the NIH then convinced the pharmaceutical giant Eli Lilly to make thousands of doses of his vaccine. Confident that he could now protect people against pneumococcus, he called the medical directors of three of South Africa's largest gold mining companies and, on September 6, 1970, flew with his wife to Johannesburg to begin talks with them. That same day, members of the Popular Front for the Liberation of Palestine hijacked four planes bound for New York. “When we got off the plane we got an effusive welcome and we couldn't figure out why,” recalled Austrian. “We were flying over North Africa when the planes were hijacked.”
Two years later, Austrian began the first test of his vaccine at the East Rand Preparatory Mine in Boksburg, fifteen miles east of Johannesburg. First established in 1893, the mine was one of the oldest and deepest in the country. Although sixty years had passed since Almroth Wright had tested his vaccine, conditions in the mines weren't much better. Austrian decided to enroll men coming to work for the first time, reasoning that they were most likely to encounter types of pneumococci not found in their isolated rural communities. “It was an unforgettable experience,” recalled Austrian, “to descend to the deepest workings of the mine two miles below the earth's surface and a mile below sea level.” Rock temperatures reached 125 degrees.
Austrian wanted to inject some miners with his pneumococcal vaccine and some with placebo. But to convince gold mine executives to use his vaccine, he had to throw in another vaccine: one against meninogococcus, a different bacterium that caused rapid, overwhelming infection. Meningococcus scared mining company officials. Workers would be fine one minute and dead four hours later. “Death gave gold mining a bad name,” recalled Austrian. “Money spent taking care of miners with pneumococcal pneumonia was just factored into the cost of the gold. But death from meningococcus was bad publicity. They let us do the [pneumococcal] study because of meningococcus.” One third of the miners received pneumococcal vaccine, one third received meningococcal vaccine, and one third received placebo. (Like the pneumococcal vaccine, the meningococcal vaccine was made from the polysaccharide coat of the bacterium.) Although he wanted to see if his vaccine saved lives, Austrian also wanted to know what levels of antibodies in blood correlated with protection against disease. This meant that he needed to collect blood samples before and after vaccination. Austrian's intellectual interest angered officials from the mining company. “We wanted to study the serological responses to the vaccine,” recalled Austrian. “The [company authorities] were willing to [allow miners to] give blood when they were acutely ill, but they objected to having their blood drawn after they'd recovered. At one point I got a call from [the authorities] that they were going to call off the trial because it was interfering with the workforce of the mine. So I got on a plane on very short notice and went back to Johannesburg, where I met with the head of one of the mining companies. I pointed out to him that the vaccine had already saved him perhaps $100,000 in terms of medical expenses.” To this, the mine owner slowly shook his head, realizing for the first time just how little Austrian knew about his business. “He looked at me, and he said that this [was] a $3 million annual operation. He wasn't interested in my problem. He had the coldest blue eyes I ever saw.” The mining executive eventually decided to let the trial continue on the condition that Austrian abandon his interest in testing blood from the miners.
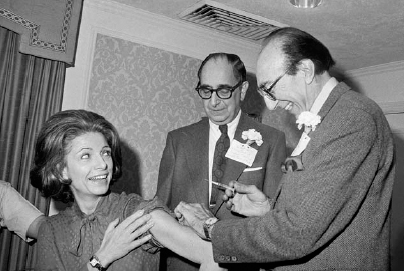
Robert Austrian (center), winner of the 1978 Lasker Award, watches Dr. Michael DeBakey inoculate Mrs. William McCormick Blair, Vice President of the Lasker Foundation, with his pneumococcal vaccine, November 20, 1978.
When the experiment was over, Austrian found that his pneumococcal vaccine worked, reducing the incidence of disease by 80 percent. Elated, he went back to the United States, certain that Eli Lilly would mass-produce the vaccine. But Lilly, which previously had been one of the largest vaccine makers in the United States, had decided to leave the vaccine business. With a vaccine in hand that could save thousands of lives, Austrian faced the very real possibility that no company would make it. In the end, only Maurice Hilleman considered Austrian's plea. “Dr. Hilleman on his own decided that Merck would make a vaccine,” recalled Austrian. “If Maurice had said âNo,' it would have all gone down the drain. I don't know of anybody else in the vaccine business who was ready to step up if Maurice hadn't supported this.”
In 1977 Maurice Hilleman and Merck made the first pneumococcal vaccine, designed to prevent infection with fourteen different types of pneumococci. In 1983 they made a second pneumococcal vaccine, containing even more different types. Austrian considers the pneumococcal vaccine to be one of the most unusual vaccines ever made. “This is probably the most complex vaccine that we have,” says Austrian. “It's designed to protect against twenty-three different infections.”
The CDC now recommends Robert Austrian's pneumococcal vaccine for people more than sixty-five years old, those most likely to die of the disease. Unfortunately, many elderly adults in the United States don't get the pneumococcal vaccine, probably our most underutilized weapon in the fight against serious, and occasionally fatal, pneumonia. Worldwide, about two million million people die of pneumococcal infections every year.