Breast Imaging: A Core Review (39 page)
Read Breast Imaging: A Core Review Online
Authors: Biren A. Shah,Sabala Mandava
Tags: #Medical, #Radiology; Radiotherapy & Nuclear Medicine, #Radiology & Nuclear Medicine
Reference: Liberman L, Drotman M, Morris EA, et al. Imaging–histologic discordance at percutaneous breast biopsy.
Cancer
2000;89(12):2538–2546.
17
Answer C.
Placing two wires with the bracketing technique is helpful in cases such as this of a larger extent of nonpalpable calcifications. This helps guide the surgeon most accurately without any guess work needed as to the extent of the disease. This technique will not ensure clean surgical margins, but it will give the surgeon the best guidance of all the options. Mastectomy will likely not be needed for a 3-cm extent of disease, so automatically cancelling the procedure would be inappropriate. Many factors do need to be considered when determining appropriateness for breastconserving therapy, including the size of the patient’s breast, the patient’s overall health, and the patient’s willingness to undergo radiation.
Reference: Liberman L, Kaplan J, Van Zee KJ, et al. Bracketing wires for preoperative breast needle localization.
AJR Am J Roentgenol
2001;177(3):565–572.
18
Answer D.
Although 14-gauge spring loaded and 14-gauge vacuumassisted biopsy devices can be used for stereotactic biopsy, they are not the most optimal or effective choice, especially when microcalcifications are the target. The false-negative rate and upgrade rates at final pathology are lower when larger core vacuum-assisted biopsy is used.
References:
ACR Practice Guideline for the Performance of Stereotactically Guided Breast Interventional Procedures
; 2009.
http://www.acr.org/~/media/62F6E5A180134DF6A014447BDEB 5384D.pdf
Jackman RJ, Burbank F, Parker SH, et al. Stereotactic breast biopsy of nonpalpable lesions: determinants of ductal carcinoma in situ underestimation rates.
Radiology
2001;218:497–502.
Jackman RJ, Marzoni FA, Rosenberg J. False-negative diagnoses at stereotactic vacuum-assisted needle breast biopsy: long-term follow-up of 1,280 lesions and review of the literature.
AJR Am J Roentgenol
2009;192(2):341–351.
19
Answer D.
Single-duct spontaneous bloody, serous, or clear nipple discharge is the only indication to perform galactography.
Reference: Shah BA, Fundaro GM, Mandava S.
Breast Imaging Review: A Quick Guide to Essential Diagnoses
. New York, NY: Springer; 2010:231.
20
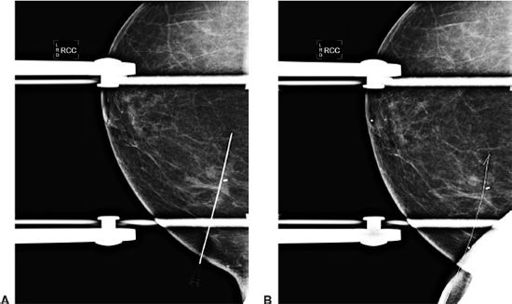
Answer C.
The orthogonal view (in our case the CC view since the needle was introduced from a medial approach) permits positioning of the needle depth (
z
coordinate). The needle tip should be 1 to 1.5 cm beyond the lesion so that the lesion remains along the needle shaft. Answer choice A is incorrect because the wire has not yet been placed and the depth has not yet been adjusted. Answer choice B is incorrect because the
x
and
y
coordinates have been confirmed and the needle tip is through the lesion. Once the relationship of the needle to the lesion has been confirmed (
x
and
y
coordinates), there is no reason to ever return to the first projection. Answer choice D is incorrect because the needle tip is 3-cm distal to the mass. The needle needs to be retracted at least 1.5 cm with the tip 1.5 distal to the mass. Answer choice C is correct. The needle tip was adjusted to the tip 1- to 1.5-cm distal to the mass, and the wire was subsequently placed (see images A and B).
Reference: Kopans DB.
Breast Imaging.
3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:924.
21
Answer D.
Answer choice A is incorrect because a specimen radiograph should be performed while the patient is still on the table with the cavity open in the operating room. The specimen radiograph helps confirm the targeted abnormality has been removed. Answer choice D is correct. Magnification radiography is preferable as it improves visualization specifically for calcifications. Answer choice C is incorrect. The radiologist looks at the lesion compared to the visible margins and alerts the surgeon if the lesion appears close to or abutting the surgical margin. However, this is not sufficient for determining surgical margins as final pathology is the gold standard. Answer choice B is incorrect. Specimen radiographs are performed for masses and calcifications. The radiologists should comment on whether the specimen contains the lesion, whether the lesion is at, is away from or is transecting the specimen edge, and whether the wire including tip and biopsy clip (if present) are included.
References: Ikeda DM.
The Requisites Breast Imaging.
St. Louis, MO: Elsevier Mosby; 2004.
Kopans DB.
Breast Imaging.
3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:927–929.
22
Answer A.
Stroke margin is the distance between where the needle tip is expected to end after firing and the distance to the far side of the breast (image receptor).
Reference: Kopans DB.
Breast Imaging.
3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:963.
23
Answer C.
Sentinel lymph node biopsy has replaced axillary dissection in patients with preoperative negative axillas. This has decreased patient morbidity. If an abnormal axillary lymph node is seen on ultrasound, it often preoperatively undergoes core needle biopsy or fine needle aspiration. If the node is metastatic, the patient undergoes axillary dissection. If the node is benign, the patient is scheduled for sentinel node biopsy at the time of surgery. A benign percutaneous biopsy of an axillary lymph node does not clear the axilla, and sentinel lymph node biopsy still needs to be performed at the time of surgery.
Reference: Kopans DB.
Breast Imaging
. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:956–957.
24
Answer D.
Stereotactic breast biopsy is performed for calcifications or a mass/asymmetry that does not have a sonographic correlate. For preprocedure planning purposes, the optimal biopsy approach is that in which the finding is closest to the skin. For example, if the suspicious finding is in the upper breast and is closest to the superior skin surface, then the optimal needle approach would be from superior approach with craniocaudal compression using a fenestrated paddle. Therefore, answer choice E is incorrect; the optimal stereotactic approach is not always lateral, but rather the approach where the finding can be reached by traversing the least distance of breast tissue. The scout image confirms that the finding is present within the fenestrated portion of the compression paddle. The stereotactic pair images are then performed at +15 degrees and −15 degrees, which the computer then uses to calculate the depth (
z
distance) of the finding based on the parallax phenomenon. In addition to calculated depth of the lesion, the computer will also inform the operator of the stroke margin. The stroke margin is the calculated distance between the needle tip and the detector once the needle has been fired. Answer choice A is incorrect. A positive (rather than a negative) stroke margin is desirable to perform the procedure. A positive stroke margin indicates that there will be enough breast tissue to accommodate the needle without traversing the entirety of the breast or damaging the detector. A compression thickness under 3 cm may not have enough breast tissue to safely accommodate the biopsy needle. A radiograph of the core specimens is performed following stereotactic biopsy to determine whether the suspicious finding has been adequately sampled. This is most commonly used for calcifications. However, it can also be used to a mass or asymmetry where pieces of focal density may be seen in the specimens. Answer choice D therefore is correct. If the finding has not been sampled adequately, biopsy sampling can continue focused to the residual finding. If the finding has been adequately sampled, then a radioopaque biopsy marker is placed. An image is taken to ensure the clip deployed, and the needle is removed with compression held to ensure hemostasis. Answer choice B is incorrect. A postprocedure mammogram is indicated to check for residual suspicious finding and the position of the biopsy marker, which can occasionally move away from biopsy site when the patient is removed from compression. Answer choice C is incorrect. Infection is a rare complication of stereotactic breast biopsy.
Reference: Cardenosa G.
Breast Imaging Companion
. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008:533–536.
25
Answer A.
The pathology and imaging findings are not concordant, and therefore a 6-month ultrasound follow-up is not an appropriate recommendation. Breast MRI or breast-specific gamma imaging (BSGI) is not indicated at this time. Regardless of the MRI or BSGI findings, a surgical excisional biopsy is required to definitely diagnose this mass. If the mass is a cancer, breast MRI or BSGI could be used for treatment planning.
Reference: Geller BM, Ichikawa LE, Buist DS, et al.; Breast Cancer Surveillance Consortium. Improving the concordance of mammography assessment and management recommendations.
Radiology
2006;241:67–75.
26
Answer B.
Relative contraindications to radiation therapy include previous radiation therapy, pregnancy, collagen vascular disease, and multicentric or diffuse disease. Axillary adenopathy is not a contraindication. Whole-breast irradiation achieves control of residual microscopic disease.
Reference: Ikeda D.
Breast Imaging: The Requisites
. 2nd ed. St. Louis, MO: Elsevier Mosby; 2011:231–233.
27
Answer A.
References: Brem RF, Schoonjans JM. Local anesthesia in stereotactic, vacuum-assisted breast biopsy.
Breast J
2001;7:72–73.
Ikeda D.
Breast Imaging: The Requisites
. 2nd ed. St. Louis, MO: Elsevier Mosby; 2011:164.
28a
Answer A.
Ductography is a procedure that can help to identify the cause of unilateral, single-pore, spontaneous nipple discharge. If an abnormality is identified, it can be targeted for surgical biopsy. Answer choice B is incorrect. Ductography is not used to biopsy an intraductal mass. Rather, ductography can be used to identify and localize a potential intraductal mass that may be causing discharge. Suspicious single-pore discharge for which ductogram is indicated includes bloody, clear/serous, or serosan-guineous discharge. These are the discharge colors that have been associated with breast cancer. White- and green-colored discharge is of benign etiology, such as physiologic or fibrocystic in nature. Therefore, answer choice C is incorrect. In order to begin the ductogram, the single-discharging pore is identified. If the discharging pore cannot be reidentified, the procedure cannot proceed. If the discharging duct is identified, a small gauge cannula tip (usually 30-gauge) is placed on the discharging duct with gentle pressure. When the cannula is in the duct, a minimal amount of contrast material is administered (0.2 to 0.3 mL). Take care to ensure that no air bubbles are present prior to injection. Therefore, answer choice D is incorrect. A dose of 5 mL is too much contrast and could cause extravasation from the duct and patient discomfort. Once the contrast is injected, the cannula is stabilized and postprocedure and magnification craniocaudal and mediolateral mammograms of the retroareolar breast are obtained.
28b
Answer D.
The patient should be referred back to a breast surgeon. In these images, an intraductal filling defect/mass is identified at the 6:00 position retroareolar. Primary differential diagnosis is papilloma or DCIS. Localizing this mass for a surgical breast biopsy will increase the probability of removing the etiology of the discharge rather than a blind surgical duct excision. The intraductal mass can be localized for subsequent surgical biopsy, either with a biopsy marker at the time of diagnostic ductogram or with a repeat ductogram/wire localization on the day of surgical biopsy. Answer choice A is incorrect. Stereotactic breast biopsy is not indicated in this instance. The standard mammogram is most likely negative, which will make the intraductal mass difficult to localize for stereotactic biopsy. Also, a percutaneous biopsy may not remove the entirety of the mass. Chances are high that this mass represents a papilloma or breast cancer, both of which would be referred to surgical excision following core biopsy. Therefore, direct referral to surgical biopsy is better for the patient. Answer choice B is not indicated. An intraductal mass that is likely contributing to the patient’s symptoms has already been identified. Breast MRI is not needed to further characterize the finding. Finally, answer choice C is incorrect. A repeat ductogram is not necessary. The filling defect in the duct in the provided images does not appear to be artifactual due to an air bubble. Artifact due to potential air bubbles tend to be round with contrast surrounding them and passing them.
Other books
Pretenders by Lisi Harrison
Growing Pains by Emily Carr
The Silencers by Donald Hamilton
A Seal Upon Your Heart by Pepper Pace
A Midnight Dance by Lila Dipasqua
Saving Sarah by Jennifer Salaiz
Cracked by K. M. Walton
Scion by McDonald, Murray
A Unique Kind of Love by Rose, Jasmine