Read Examination Medicine: A Guide to Physician Training Online
Authors: Nicholas J. Talley,Simon O’connor
Tags: #Medical, #Internal Medicine, #Diagnosis
Examination Medicine: A Guide to Physician Training (76 page)
6.
Left ventricular failure (a late sign – right ventricular failure is preterminal).
RESULTS OF INVESTIGATIONS
1.
ECG – left ventricular hypertrophy (systolic overload).
2.
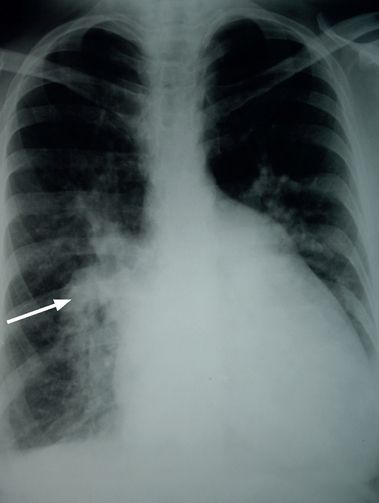
Chest X-ray film (see
Fig 16.12
):
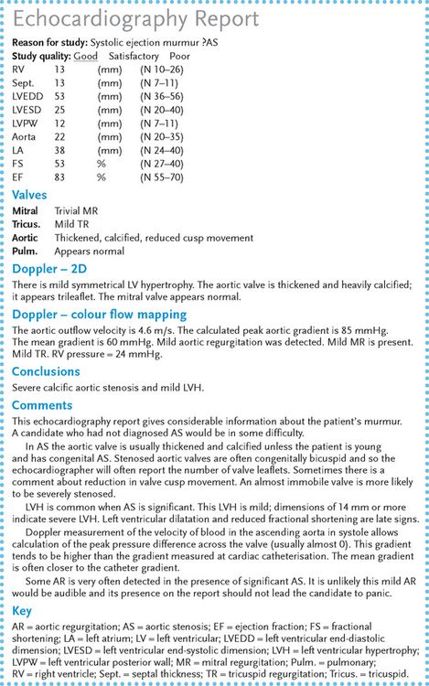
FIGURE 16.12
Chest X-ray of a patient with calcific aortic stenosis; valve calcification is visible (arrow). Figure reproduced courtesy of The Canberra Hospital.
a.
left ventricular hypertrophy
b.
valve calcification.
3.
Echocardiography (see
Fig 16.13
):
FIGURE 16.13
Echocardiography report for a patient with aortic stenosis.
a.
Doppler estimation of gradient (
note:
Doppler estimation of peak gradient usually overestimates the value compared with cardiac catheterisation)
b.
valve cusp mobility
c.
left ventricular hypertrophy
d.
left ventricular dysfunction.
INDICATIONS FOR SURGERY
1.
Symptoms – exertional angina, exertional dyspnoea, exertional syncope (urgent).
2.
Critical obstruction (based on catheterisation data) and severe left ventricular hypertrophy even if asymptomatic.
CHOICE OF VALVE
Tissue (bovine pericardial or porcine, or occasionally homograft) valves are usually offered to patients over the age of about 65 or to younger patients who wish to avoid warfarin. Their life expectancy before failing is up to 15 years or more.
Tricuspid regurgitation
Look for the following signs:
1.
the JVP – large
v
waves: the JVP is elevated if right ventricular failure has occurred
2.
palpation – right ventricular heave
3.
auscultation – a pansystolic murmur, maximal at the lower end of the sternum and on inspiration, may be present, but the diagnosis can be made on the basis of the peripheral signs alone; multiple systolic clicks are characteristic of Ebstein’s anomaly of the tricuspid valve
4.
abdomen – a pulsatile, large and tender liver is usually present; ascites and oedema with pleural effusions may also occur.
CAUSES
1.
Functional (no disease of the valve leaflets) – right ventricular failure.
2.
Rheumatic – only very rarely does tricuspid regurgitation occur alone; usually mitral valve disease is also present.
3.
Infective endocarditis (right-sided endocarditis in intravenous drug abusers).
4.
Congenital – Ebstein’s anomaly.
5.
Tricuspid valve prolapse (rare).
6.
Right ventricular papillary muscle infarction.
7.
Trauma (usually a steering-wheel injury to the sternum).
RESULTS OF INVESTIGATIONS
The chest X-ray film may show right ventricular enlargement or biventricular enlargement if the tricuspid regurgitation is secondary to heart failure. Patients with Ebstein’s anomaly may have the characteristic box-shaped heart and narrow cardiac base (see
Fig 16.14
). Echocardiography enables detection of structural valve abnormality and
estimation of the size of the regurgitant jet in the right atrium. Measurement of the velocity of this jet allows estimation of the pressure gradient across the valve. As right atrial pressure is usually 5–10 mmHg, the right ventricular pressure can be estimated in any patient with tricuspid regurgitation by adding 5 to this pressure gradient. Trivial tricuspid regurgitation is a common and normal Doppler echocardiogram finding.
FIGURE 16.14
Chest X-ray of a patient with Ebstein’s anomaly, showing a narrow cardiac pedicle. Figure reproduced courtesy of The Canberra Hospital.
Pulmonary stenosis (in adults)
Look for the following signs:
1.
general signs
a.
peripheral cyanosis because of a low cardiac output
b.
the pulse – normal or reduced because of a low cardiac output
c.
the JVP – giant
a
waves because of right atrial hypertrophy; the JVP may be elevated
d.
palpation – right ventricular heave; thrill over the pulmonary area (common)
e.
auscultation – the murmur may be preceded by an ejection click; a harsh ejection systolic murmur maximal in the pulmonary area and on inspiration is present; S4 may be present (owing to right atrial hypertrophy)
f.
abdomen – presystolic pulsation of the liver may be present
2.
signs of severe pulmonary stenosis
a.
an ejection systolic murmur peaking late in systole
b.
absence of an ejection click (also absent when the pulmonary stenosis is infundibular, i.e. below the valve level)
c.
presence of S4
d.
signs of right ventricular failure.
CAUSES
1.
Congenital.
2.
Carcinoid syndrome.
Chronic constrictive pericarditis
This is a difficult diagnosis, the clue is often that the patient appears cachectic and has ascites. Look for the following signs:
1.
pulse and blood pressure – a low blood pressure and pulsus paradoxus are typical
2.
JVP – this is raised; Kussmaul’s sign is rare; the
x
and
y
descents are prominent
3.
apex beat – impalpable
4.
heart sounds – these are distant; there may be an early third heart sound and an early pericardial knock (as rapid ventricular filling is abruptly halted)
5.
hepatosplenomegaly, ascites and oedema provide important clues
6.
underlying aetiology (e.g. radiation, tumour, tuberculosis, connective tissue disease, chronic renal failure, trauma).
Hypertrophic cardiomyopathy
It is always important to consider this diagnosis – it is a popular ‘trap’! The classical signs are as follows:
1.
Pulse – this is typically sharp, rising and jerky, owing to rapid ejection by a hypertrophied ventricle early in systole, followed then by obstruction; it is not like the pulse of aortic stenosis.
2.
The JVP – there is a prominent
a
wave owing to forceful atrial contraction against a non-compliant ventricle.
3.
Apex beat – there is typically a double or triple impulse owing to presystolic ventricular expansion following atrial contraction.
4.
Auscultation:
a.
late systolic ejection murmur (left sternal edge)
b.
pansystolic murmur (apex) from mitral regurgitation
c.
fourth heart sound.
Note:
there are no diastolic murmurs.
5.
Dynamic manoeuvres – the murmur is louder with the Valsalva manoeuvre, standing and isotonic exercise (e.g. jogging – not usually possible under examination conditions). The murmur is softer with squatting, raising the legs and isometric exercise (e.g. forceful handgrip).
RESULTS OF INVESTIGATIONS
1.
ECG:
a.
left ventricular hypertrophy and lateral ST segment and T wave changes
b.
deep Q waves
c.
conduction defects.
2.
Chest X-ray film:
a.
left ventricle enlarged with a hump along the border
b.
no valve calcification.
3.
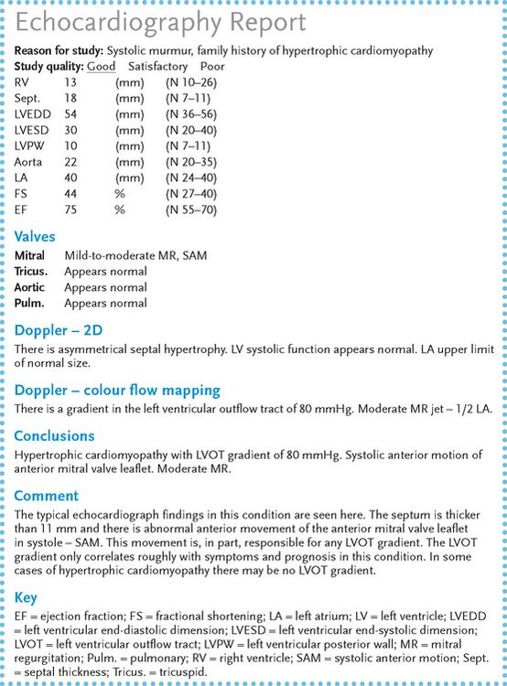
Echocardiography (see
Fig 16.15
):
FIGURE 16.15
Echocardiography report for a patient with hypertrophic cardiomyopathy.
a.
asymmetrical hypertrophy (ASH) of the ventricular septum
b.
systolic anterior motion (SAM) of the anterior mitral valve leaflet
c.
midsystolic closure of the aortic valve
d.
Doppler detection of mitral regurgitation
e.
Doppler estimation of the gradient in the left ventricular outflow tract.
Non-cyanotic congenital heart disease
These are difficult examination cases that not infrequently crop up in the test.
ATRIAL SEPTAL DEFECT
There are two types (sinus venosus defects are not often seen in adults): ostium secundum and ostium primum.
ASD: ostium secundum
This is the most common and presents in adult life with:
1.
fixed splitting of the second heart sound (
note:
unfortunately, an ASD is still a possible diagnosis when some variation in splitting is detectable during the respiratory cycle)
2.
pulmonary systolic ejection murmur (increasing on inspiration)
3.
pulmonary hypertension (late).
Results of investigations
1.
ECG:
a.
right-axis deviation
b.
right bundle branch block pattern
c.
right ventricular hypertrophy (systolic overload).
2.
Chest X-ray film (see
Fig 16.16
):