i bc27f85be50b71b1 (115 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown
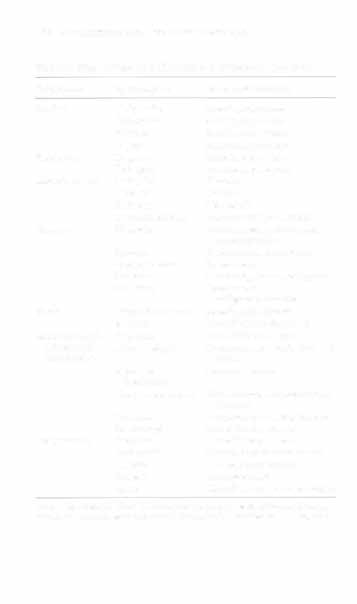
Table 6-5. Continued
w
:;!
Test
Description
:>
Ankle-brachial index (ABI)
Systolic blood pressures are taken in both upper extremities at the brachial arter
§
ies and both lower extremities above the ankle, followed by Doppler evaluation of dorsalis pedis or posterior tibialis pulses. The higher of the lower
§
extremity pressures is rhen divided by the higher of rhe upper-extremity pres
�
sures (e.g., an ankle pressure of 70 mm Hg and a brachial pressure of 140 mm
"
Hg will yield an AB) of 0.5).
g
Normal ASI for foO[ arteries is 0.95-1.20. with indexes below 0.95 indicating
"
arterial obstruction.
2l
"
Exercise testing
Exercise testing is performed to assess the nature of claudication by measuring
�
ankle pressures and PVRs after exercise.
J:
-<
�
A drop in ankle pressures can occur with arterial disease.
�
This type of testing provides a controlled method to document onset. severity,
r
and location of claudication.
i
!il
Screening for cardiorespiratory disease can also be performed, as patients with
:>
peripheral vascular disease often have concurrent cardiac or pulmonary disor
�
ders (see Chapter I).
Computed tomography (CT)
CT is used ro provide visualization of the arterial wall and its Structures.
Indications for CT include diagnosis of abdominal aortic aneurysms and pOStoperative complications of graft infections, occlusions, hemorrhage, and abscess.


Magnetic resonance imaging (MRI)
MRI has multiple uses in evaluating the vascular system and is now morc commonly used to visualize the arterial system than arteriograms. Specific uses for MRI include detection of deep venous thrombosis and evaluation of cerebral
edema.
Serial MRls can also be used to help detemline me optimal operative time for patients
with cerebrovascular accidents by monitoring their progression.
Magnetic resonance angiography
MRA uses blood as a physiologic contrast medium to examine the structure
(MRA)
and location of major blood vessels and the flow of blood through these vessels. The direction and rate of flow can also be quantified. MRA minimizes complications that may be associated with contrast medium injection.
Sources: Data from JM Black, E l\tatassarin-Jacobs (cds). Luckmann and Sorensen's Medical-Surgical Nursing: A PsychophYSiOlogic Approach (4th cd). Philadelphia: Saunders, 1993; P Lanzer, J Rosch (cds). Vascular Diagnostics: Noninvasive and Invasive Techniques, Peri-Interventional Evaluations. Berlin: Springer-Verlag, 1994; KL McCance, SE Huether (cds). Pathophysiology: The Biological Basis for Disease in Adults and Children (2nd ed). St. Louis: Mosby, 1994; JL Kee (cd). Laboratory and Diagnostic Tests with Nursing Impli
�
cations (5th cd). Stamford: Appleton & Lange, 1999,606; VA Fahey (cd). Vascular Nursing (3rd ed). Philadelphia: Saunders, 1999j76, r;:
86; and LM Malarkey, ME Morrow (cds). Nurses Manual of Laboratory Tests and Diagnostic Procedures (2nd ed). Philadelphia: Saun
"
den. 2000;359.
� )-�
J:
�
@
g
-<
w
�

376 Acme CARE HANDBOOK FOR PHYSICAL THERAJlISTS
•
Frequent vital sign monitoring with pulse assessments.
•
If a patient has been on heparin before angiography, the drug is
not resumed for a minimum of 4 hours.s
The following are complications associated with angiography,·s.6:
•
Allergic reactions to contrast dye
• Thrombi formation
• Vessel perforation with or without pseudoaneurysm formation
• Hematoma formation
• Hemorrhage
•
Infections at the injection site
• Neurologic deficits from emboli dislodgment
• Contrast-induced renal failure (refer to Chapter 9)
Hematologic Evaluation
The medical work-up of the patient with a suspected hematologic
abnormality emphasizes the patient history and laboratory studies, in
addition to the patient's clinical presentation.
History
In addition to the general charr review (see Appendix I-A), the following questions are especially relevant in the evaluation of the patient with a suspected hematologic disorder7-':
• What are the presenting symptoms?
• Was the onset of symptoms gradual, rapid, or associated with
trauma or other disease?
•
Is the patient unable to complete daily activities secondary to
fatigue?
•
Is there a patient or family history of anemia or other blood disorders, cancer, hemorrhage, or systemic infection?
•
Is there a history of blood transfusion?

VASCULAR SYSTEM AND HEMATOLOGY
377
•
Is there a history of chemotherapy, radiation therapy, or other
drug therapy?
• Has there been an environmental or occupational exposure to
toxins?
• Have there been night sweats, chills, or fever?
• Is the patient easily bruised?
• Is wound healing delayed?
• Is there excessive bleeding or menses?
Other relevant data include rhe patient's diet (for the evaluation of
vitamin- or mineral-deficiency anemia), history of weight loss (as a
warning sign of cancer or altered metabolism), whether the patient
abuses alcohol (a cause of anemia with chronic use), and race
(some hematologic conditions have a higher incidence in certain
races)_
Inspection
During the hematologic evaluation, the patient is observed for the
following7:
• General appearance (for lethargy, malaise, or apathy)
•
Degree of pallor or flushing of the skin, mucous membranes,
nail beds, and palmar creases
• Presence of petechiae (purplish, round, pinpoint, nonraised
spotS caused by intradermal or subcuraneous hemorrhage)'o or
ecchymosis (bruising)
• Respiratory rate
Palpation
The examination performed by rhe physician includes palpation
of lymph nodes, liver, and spleen as parr of a general physical
examination. For specific complaints, the patient may receive
more in-deprh examinarion of a body system. Table 6-6 summarizes rhe abnormal hematologic findings by body system on physical examinarion. The physical rherapist may specifically examine the following:
378 AClITE CARE HANDBOOK FOR PHYSICAL THERAPISTS
Table 6-6. Signs and Symproms of Hematologic Disorders by Body System
Body System
Sign/Symptom
Associated Condition
Cardiac
Tachycardia
Anemia, hypovolemia
Palpitations
Anemia, hypovolemia.
Murmur
Anemia, hypovolemia
Angina.
Anemia, hypovolemia
Respirarory
Dyspnea
Anemia, hypovolemia
Orthopnea
Anemia, hypovolemia
Musculoskeletal
Back pain
Hemolysis
Bone pain
Leukemia
Joint pain
Hemophilia
Sternal tenderness
Leukemia, sickle-cell disease
Nervous
Headache
Severe anemia, polycythemia,
metastatic tumor
Syncope
Severe anemia, polycythemia
Vertigo, tinnitus
Severe anemia
Paresthesia
Vitamin BI1 anemia, malignancy
Confusion
Severe anemia,
malignancy, infection
Visual
Visual disturbances
Anemia, polycythemia
Blindness
Thrombocytopenia, anemia
Gastrointestinal,
Dysphagia
Iron-deficiency anemia
urinary, and
Abdominal pain
Lymphoma, hemolysis, sickle-cell
reproductive
disease
Spleno- or
Hemolytic anemia
hepatomegaly
Hematemesis, melena Thrombocytopenia and clotting
disorders
Hematuria
Hemolysis and clotting disorders
Menorrhagia
Iron-deficiency anemia
Integumentary
Petechiae
Iron-deficiency anemia
Ecchymosis
Hemolytic, pernicious anemia
Flushing
Iron-deficiency anemia
Jaundice
Hemolytic anemia
Pallor
Conditions with low hemoglobin
Source: Data from JM Bbck, E Matassarin-Jacobs (eds). Medical-Surgical Nursing
Clinical Management for Conrinuity of Care (5th cd). Philadelphia: Saunders, 1997.