i bc27f85be50b71b1 (127 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown
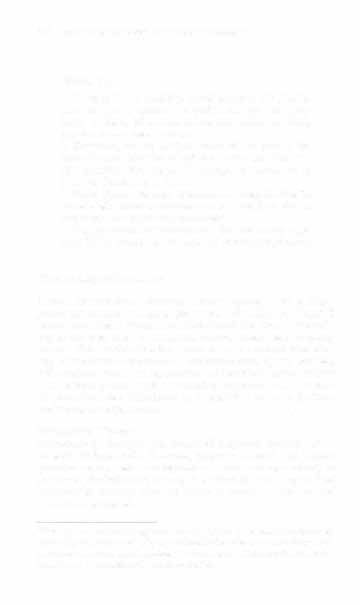
Table 6-15. Common Blood Products and Their Clinical Indications and Omcomes
Product
Content
Clinicallndications
Outcome
Whole blood
Blood cells and
Acme major blood loss in setting of
Resolution of signs and symptoms of
plasma
hypotension, tachycardia, tachypnea,
hypovolemic shock or anemia.
pallor, and decreased Hct and Hgb.
Hct should increase 3% in a non bleeding
To treat oxygen-catrying deficit (RBC) and
adult (per unit transfused).
volume expansion (plasma).
Whole blood is rarely used.
Red blood cells
RBCs only
Acute or chronic blood loss.
Resolution of signs and symptoms of
(RBCs)
To treat oxygen-carrying deficit in sccring
anemia.
of tachycardia, tachypnea, pallor,
Hct should increase 3% in a nonbleeding
<
faeigue, and decreased Hct and Hgb.
adult (per unit transfused).
Anemia without need for volume
§
expansion.
i:
"
Plaeelets (Pits)
Concentrated Pits
To restore clotting function associatcd
Resolution of thrombocytopenia.
�
in plasma
with or a&er blood loss.
Prevention or resolution of bleeding.
�
To increase Pit coune in a bleeding patient
Pit should increase 5,000 in a lO-kg adult
with Pit < 1 00,000, in advance of a pro
(per unie).
,.
z
"
cedure with Pit <50,000, or prophylacti
:r
cally wieh Pic <10,000.
�
� g -<
...
�
"

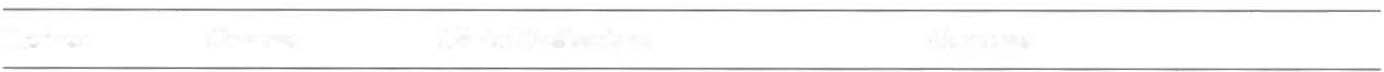
Table 6-15. Continued
...
-
00
Product
Content
Clinical Indications
Outcome
>-
n
Fresh-frozen
All plasma
To replace or increase coagulation factor
Improved or adequate coagulation lev-
�
plasma (FFP)
components,
levels.
els or factor assays.
n
>
'"
namely blood
Acute disseminated intravascular coagu-
'"
factors and pro-
lopathy.
J:
>-
tein
Thrombotic thrombocytopenic purpura.
z
"
=
Factor Xl deficiency.
0
0
Rapid reversal of warfarin therapy.
"
"
Albumin
Albumin cells
Volume expansion in situations when crys-
Acquire and maintain adequate blood
'"
�
with few globu-
ralloid (saline or Ringers lactate) is inad-
pressure and volume support.
J:
-<
lins and other
equate such as shock, major hemor-
R
proteins
rhage, or plasma exchange.
>-
r
Acute liver failure.
""
J:
m
Burn injury.
'"
>-
Plasma protein
Albumin,
See Albumin, above.
See Albumin, above.
�
"i
fraction
globulins, and
�
(PPF)
plasma proreins

Cryoprecipitate
Factors VIII and
Rcplacemenr of these factor deficiencies.
Correction of these faeror or fibrinogen
XlII, von WiUe
Replacement of fibrinogen when an
deficiencies.
brand's factOr,
increase in volume would not be toler
Cessation of bleeding in uremic patients.
and fibrinogen
ared with FFP.
in plasma
Bleeding associated with uremia.
Her = hematocrit, Hgb = hemoglobin.
Sources: Data from National Blood Resource Education Programs Transfusion Therapy Guidelines for Nurses. US Depanmem of Health and Human Services, National Institutes of Health, September 1990; and adapted from WH Churchill. Transfusion Therapy. New York: Sciemific American Medicine, 2001 ;4.
;;
§
<;
'"
�
-<
� >Z "
� g -<
..
�
'"

Table 6-16. Acute Adverse Blood Reactions
...
'"
o
Reaction
Cause
Signs and Symptoms
>
Febrile reaction
Patienr's blood (antileukocyte antibod
Low-grade fever, headache, chills, flushed
�
ies) is sensitive to transfused plasma
skin, muscle pain, anxiety (mild)
�
protein, platelets, or white blood
Hypotension, tachycardia, tachypnea,
i::
cells.
cough (severe)
Onset: during transfusion or up to 24 hrs
�
post transfusion
13
Allergic reaction
Patient's blood (lgE, IgG, or both) is sen11
Hives, flushed or itchy skin, and bronchial
sitive
o
[0 transfused plasma protein.
wheezing (mild)
'"
Tachypnea, chest pain, cardiac arrest
�
:r
(severe)
�
Onset: within minutes of transfusion
Q
Septic reaction
r
Transfused blood components arc con
Rapid onset of high fever, hypotension,
:i!
taminated with bacteria.
chills, emesis, diarrhea, abdominal
!il
cramps, renal failure, shock
>
�
Onset: within minutes ro 30 mins after
�
transfusion
Acute hemolytic reaction
Patient's blood and transfused blood
Tachycardia, hypotension, tachypnea,
are not compatible, resulting in red
cyanosis, chest pain, fever, chills,
blood cell destruction.
head- or backache, acute renal failure, cardiac arrest
Onset: within minutes to hours afrer
transfusion

Anaphylacric reaction
Patient is deficient in IgA and develops
Hives (mild)
IgA antibody to transfused compo
Wheezing or bronchospasm, an.xiery,
nents.
cyanosis, nausea, emesis, bloody
diarrhea, abdominal cramps, shock,
cardiac arrest (severe)
Onset: within a few seconds after exposure
Ig = immunoglobulin.
Sources: Adapted from B Kozier, G Erb, K Blais, JM Wilkinson (cds). Fundamentals of Nursing: Concepts, Process and Practice (5rh cd).
Redwood Cit)', CA. Benjamin-Cummings, 1995;110; and data from PJ Larison, LO Cook. Adverse Effects of Blood Transfusion. In OM
Harmening (cd), Modern Blood Banking and Transfusion Practices. Philadelphia: FA DavIs, 1999; and Narional Blood Resource Education Programs Transfusion Therapy Guidelines for Nurses. US Department of J-Iealrh and Human Services, Nadonal lnsritures of Health.
<
Seprember 1990.
§ � '"
�
o
:l!
,.
Z
"
� 5 CJ -<
...
N
�