i bc27f85be50b71b1 (129 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown
VASCULAR SYSTEM AND HEMATOLOGY 425
J
l
�
c
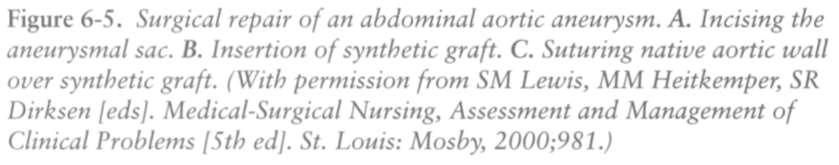
Figure 6-4. Aortofemoral graft. A. Schematic illustration of a preoperative
aortogram. B. A segment of diseased aorta is resected, and the distal aortic
stump is oversellJII. C. End-to-end proximal anastomosis. D. Completed
reconstruction. (With permission from RB Rutherford led]. Vascular Surgery
[5th ed[. Philadelphia: Sal/llders, 2000;951.)
•
Pseudoaneurysm formation at the anastomosis
•
Infection
•
Renal failure
•
Sexual dysfunction
•
Spinal cord ischemia
•
Colon ischemia
Endarterectomy
Endarterectomy is a process in which the stenotic area of an artery
wall is excised and the noninvolved ends of the artery are reanastomosed. It can be used to correct localized occlusive vascular disease, commonly in the carotid arteries, eliminating the need for bypassing the areaB



426
ACUTE CARE HANDBOOK FOR PHYSICAL THE.RAPISTS
Clinical Tip
The abbreviation CEA is often used to refer to a carotid
endarterectomy procedure.
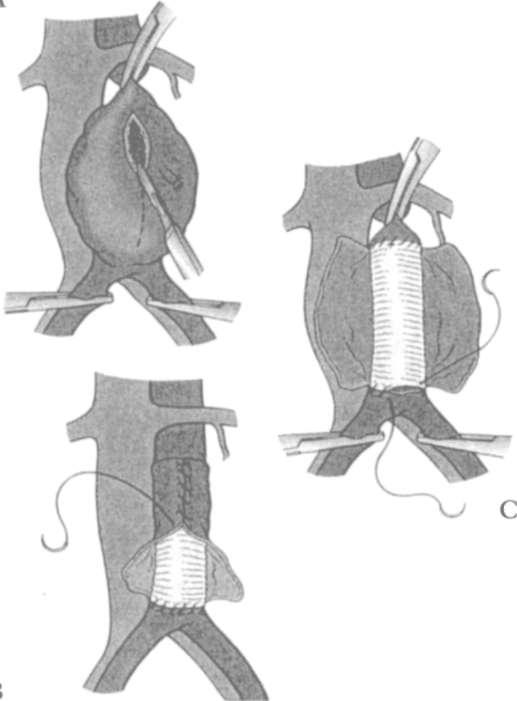
Aneurysm Repair and Reconstruction
Aneurysm repair and reconstruction involve isolating the aneurysm
by clamping off the vessel proximal and distal to the aneurysm, excising the aneurysm, and replacing the aneurysmal area with a synthetic graft. Performing the procedure before the aneurysm ruptures (elective surgery) is preferable to repairing a ruptured aneurysm (emergency surgery), because a ruptured aneurysm presents an extremely challenging and difficult operative course owing to the hemodynamic
instability from hemorrhage. The cross-clamp time of the vessels is
also crucial, because organs distal to the site of repair can become
ischemic if the clamp time is prolonged. Complications that may
occur after aneurysm repair are similar to those discussed in Peripheral Vascular Bypass Grafting' Figure 6-5 illustrates an aneurysm repair and reconstruction.
Clinical Tip
•
Incisions should be inspected before and after physical
therapy interventions to assess the patency of the incision,
as drainage or weeping may occur during activity. If drainage or weeping occurs, stop the current activity and
inspect the amount of drainage. Provide compression, if
appropriate, and notify the nurse promptly. Once the
drainage is stable or under the management of the nurse,
document the incidence of drainage accordingly in the
medical record.
•
Abdominal incisions or other incisional pain can limit a
patient's cough effectiveness and lead to pulmonary infection. Diligent attention to position changes, deep breathing, assisted coughing, and manual techniques (e.g., percussion and vibration techniques as needed) can help
prevent pulmonary infections.
•
Grafrs rhat cross rhe hip joint, such as aortobifemoral
grafts, require clarification by the surgeon regarding the
amount of flexion allowed at the hip.



• After a patient is cleared for out-of-bed activity, specific
orders from the physician should be obtained regarding
weight bearing on the involved extremities, particularly
those with recent bypass grafts.
• Patients may also have systolic blood pressure limita-
tions postoperatively to maintain adequate perfusion of
the limb or to ensure the patency of the graft area.
Blood pressures that are below the specified limit may
decrease perfusion, whereas pressures above the limit
may lead to graft damage. Thorough vital sign monitor-
ing before, during, and after activity is essential.7

428
AClITE CARE HANDBOOK FOR PHYSICAL THERAPISTS
• Patients who are status post bypass grafting procedures
should have improved peripheral pulses; therefore, any
reduction in the strength of distal peripheral pulses that
occurs after surgery should be brought to the attention of
the nurse and physician.
Physical Therapy Interventions for Patients with Vascular and
Hematologic Disorders
The primary goal of physical therapy for patients with vascular and
hematOlogic disorders is the optimization of functional mobililry and
activity tolerance. In addition to these goals, patients with vascular
disorders require patient education to prevent skin breakdown and
DVT formation, manage edema, and prevent joint contractu res and
muscle shortening. Patients with hematOlogic disorders may require
patient education for activity modification, pain management, or fall
prevention (especially if the patient is at risk of bleeding or on anticoagulant therapy).
Guidelines for the physical therapist working with the patient who