i bc27f85be50b71b1 (21 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown
ablation of plaques without thermal injury to the vessel. The laser treatment results in a more pliable lesion that responds better to balloon expansion. The use of laser angioplasty is limited owing to the expense
of the equipment and a high restenosis rate (>40%).·5
3.
Directional coro/wry atherectomy can be performed by
inserting a catheter with a currer housed at the distal end on one
side of the catheter and a balloon on the other side.12 The balloon
inflates and presses the cutter against the atheroma (plaque). The
cutter can then cut the atheroma and remove it from the arterial
wall. This can also be performed with a laser on the tip of the
catheter. Rotational ablation uses a high-speed rotating bur coated
with diamond chips, creating an abrasive surface. This selectively
removes atheroma due to its inelastic properties as opposed to the
normal elastic tissue. 12 The debris emitted from this procedure is
passed into the coronary circulation and is small enough to pass
52 ACUTE CARE HANDBOOK FOR PHYSICAL THERAPISTS
through the capillary beds. Commonly, PTCA is used as an adjunct
to this procedure to increase final coronary diameter or ro allow
for stent placemenr.
4.
Elldaillmillal stents are tiny spring-like tubes that can be
placed permanently inro the coronary artery ro increase the intraluminal diameter. Stems are occasionally necessary when initial attempts at revascularization (e.g., angioplasty) have failed.12
Clinical Tip
Refer to the Diagnostic and Laboratory Section's discussion for precautions after a catheterization procedure.
Transmyocardial Revascularization
[n transmyocardial revascularizarion, a catheter with a laser tip creates
transmural channels from patent coronary arteries into an area of the
myocardium that is thought to be ischemic. It is intended for patients
with chronic angina who, due to medical reasons, cannot have angioplasty or CABG. Theoretically, ischemia is reduced by increasing the amount of oxygenated blood in ischemic tissue. Angiogellesis (the
growth of new blood vessels) has also been proposed as a mechanism
of improvement after this procedure. Although therapists should expect
improvements in functional capacity with decreased angina, the
patient's risk status related to CAD or left ventricular dysfunction does
not change.46 Postcatheterization procedure precautions, as previously
described, will apply after this procedure.
Coronary Artery Bypass Graft
A CASG is performed when the coronary artery has become completely occluded or when it cannot be corrected by PTCA, coronary arrhrecromy, Or stenting. A vascular graft is used to revascularize the
myocardium. The saphenolls vein and the left internal mammary
artery are commonly used as vascular grafts. CABG can be performed either through a median sternotomy, which extends caudally from JUSt inferior to the suprasternal notch to below the xiphoid
process and splits the sternum longitudinally, or through a variety of
minimally i nvasive incisions.12
A minimally invasive technique that is being used for CASG
includes a CASG with a median sternoromy but without coronary
CARDIAC SYSTEM
53
bypass (off-pump CASG). This procedure eliminates the need for
cross clamping the aorta and is desirable in patients with left ventricular dysfunction or with severe atheroscierosis.12
If a median sternotomy is performed instead of the minimally
invasive incisions, then patients are placed on sternal precautions
for at least 8 weeks. They should avoid lifting of moderate to heavy
weights (e.g., greater than 1 0 Ib) with the upper extremities.
Clinical Tip
• To help patients understand this concept, inform them
that a gallon of milk weighs approxminately 8.5 lb.
•
Because of the sternal incision, patients are at risk of developing pulmonary complications after a CABG. The physical
therapist should be aware of postoperative complication risk
facrors as well as postoperative indicators of poor pulmonary
function. Refer to Chapter 2 and Appendix V for furrher
description of postoperative pulmonary complications.
Ablation Procedure
Catheter ablation procedures are indicated for supraventricular tachycardia, AV nodal re-entrant pathways, atrial fibrillation, atrial flurrer, and some patients with cerrain types of ventricular tachycardia. 12 The procedure anempts to remove or isolate ectopic foci in an attempt to reduce the resultant rhythm disturbance. Radiofrequency ablation uses lowpower, high-frequency AC current to destroy cardiac tissue and is the most effective technique for ablation.12 After the ecropic foci are located
under fluoroscopic guidance, the ablating catheter is positioned at the site
to deliver a current for 10-60 seconds.
Clinical Tip
•
Aftet an ablation procedure, the leg used for access
(venous puncture site) must remain straight and immobile for
3-4 hours. If an arrery was used, this time generally increases
to 4-6 hours. (The exact time will depend on hospital policy.)
•
Patients are sedated during the procedure and may
require time after the procedure to recover.


S4 AClJH. CARE HANDBOOK FOR I)HYSICAL THERAPISTS
• MOSt of the postintervenrion care is geared toward
moniroring for complications. Possible complications
include bleeding from the access site, cardiac tamponade
from perforation, and arrhythmias.
• After a successful ablation procedure (and the initial
immobility to prevent vascular complications at the access
site), there are usually no activity restrictions.
Cardiac Pacemaker Implantation and Automatic Implantable
Cardiac Defibrillator
Cardiac pacemaker implanration involves the placement of a unipolar or
bipolar electrode on the myocardium. This electrode is used to create an
action potential in the management of certain arrhythmias. Indications
for cardiac pacemaker implantation include the following'2•47.48:
• Sinus node disorders (bradyarrhythmias [HR lower than 60 bpmJ)
• Atrioventricular disorders (complete heart block, Mobitz
type 11 block)
• Tachyarrhythmias (supraventricular tachycardia, frequent ectopy)
Temporary pacing may be performed after an acute MI to help
control transient arrhythmias and after a CABG. Table 1 - 1 9 classifies
the various pacemakers.
One of the most critical aspects of pacer function for a physical therapist to understand is rate modulation. Rate modulation refers ro the pacer's ability to modulate HR based on activity or physiologic
demands. Not all pacers are equipped with rate modulation; therefore,
some patients have HRs that may not change with activity. In pacers
with rate modulation, a variety of sensors are available to allow adjustment of HR. The type of sensor used may impact the ability of the pacer to respond to various exercise modalities. For more detail, the
teader is teferred to the review by Sharp 48
Clinical Tip
• If the pacemaker does not have rate modulation, lowlevel activity with small increases in metabolic demand is
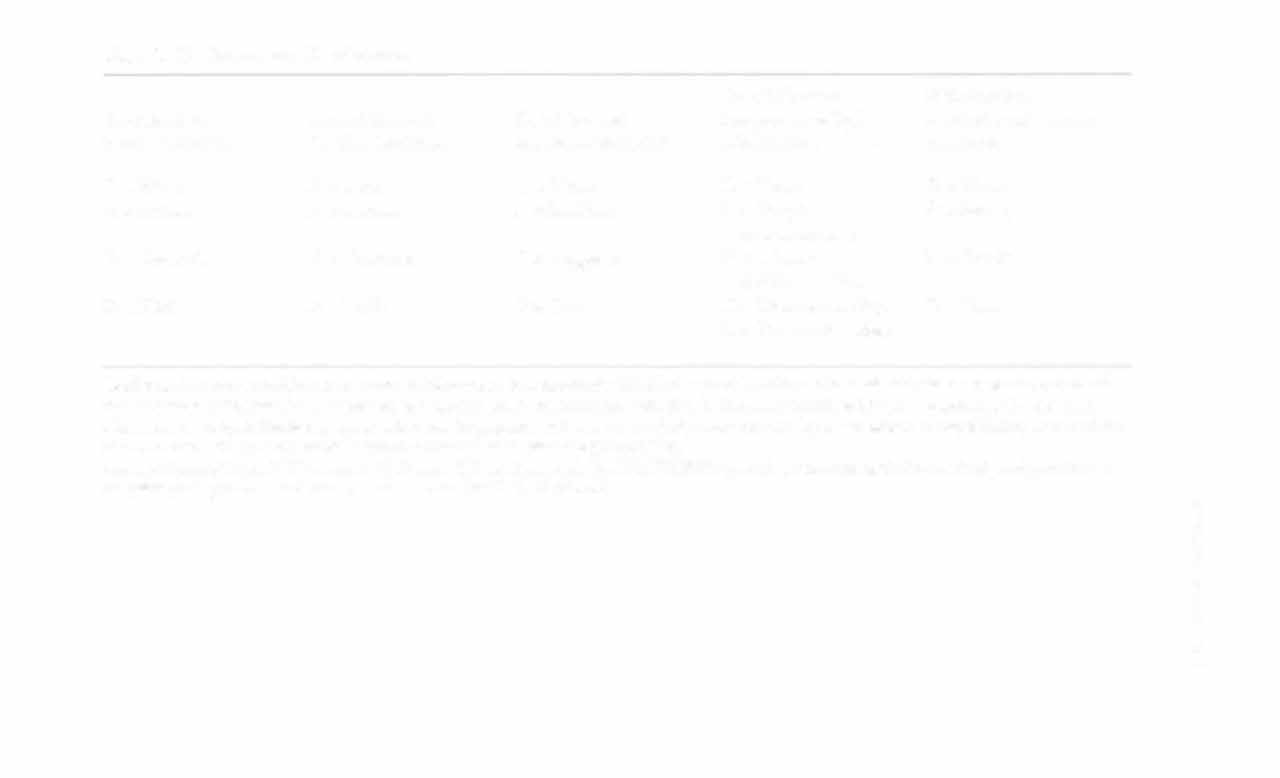

Table 1-19. Pacemaker Classification
Fourth Symbol
Fifth Symbol
First Symbol
Second Symbol
Third Symbol
Programma biliry/
Antitachyarrhythmia
Pacing Location
Sensing LOC3[ion
Response to Pacing