i bc27f85be50b71b1 (23 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown
long period of convalescence both before and after surgery, rendering them deconditioned. In general, heart transplant patients are immunosuppressed and are without neurologic input to their
heart. These patients rely first on the Frank-Starling mechanism to
augment SV and then on the catecholamine response to augment
both H R and SV. The reader is referred to Chapter 12 for information on heart and heart-lung transplantation.
Cardiac Medications
Cardiac medications are classified according to functional indications, drug classes, and mechanism of aerion. Cardiac drug classes are occasionally indicated for more rhan one clinical diagnosis.
CARDIAC SYSTEM
59
The primary functional indications and descriptions are provided
below. Appendix IV lists the functional indications, mechanisms of
action, side effects, and the generic (trade names) of these cardiac
medications.
Anti-Ischemic Medications
Anti-ischemic drugs attempt ro re-establish the balance between myocardial oxygen supply and demand.' To balance the supply and demand, medications can decrease HR or systemic BP or increase
arrerial lumen size by decreasing spasm or thrombus.
Medications that are successfully used for this task include the
followingSo:
• Beta-blockers (see Appendix Table lV- 1 2 )
• Calcium channel blockers (see Appendix Table lV- 1 4)
• Nitrates (smooth muscle cell selective) (see Appendix Table lV-24)
• Thrombolytic agents (see Appendix Table lV-29)
• Antiplatelet and anticoagulation agents (see Appendix Tables
IV- l O and IV-4, respectively)
Medications for Congestive Heart Failure
Heart failure treatment may include oral medications for a low-level
chronic condition or intravenous medications for an acute and lifethreatening condition. Medical management generally attempts ro improve the pumping capability of the heart by reducing preload,
increasing contractility, reducing afterload, or a combination of these.
Medication classes successful in achieving these goals include the
foliowingSo:
• Diuretics (see Appendix Table lV- l 7)
• Positive inotropes (see Appendix Table lV-27.A,B)
• Vasodilarors (sec Appendix Table IV-30)
• Angiotensin-converting enzyme inhibirors (see Appendix Table lV-2)
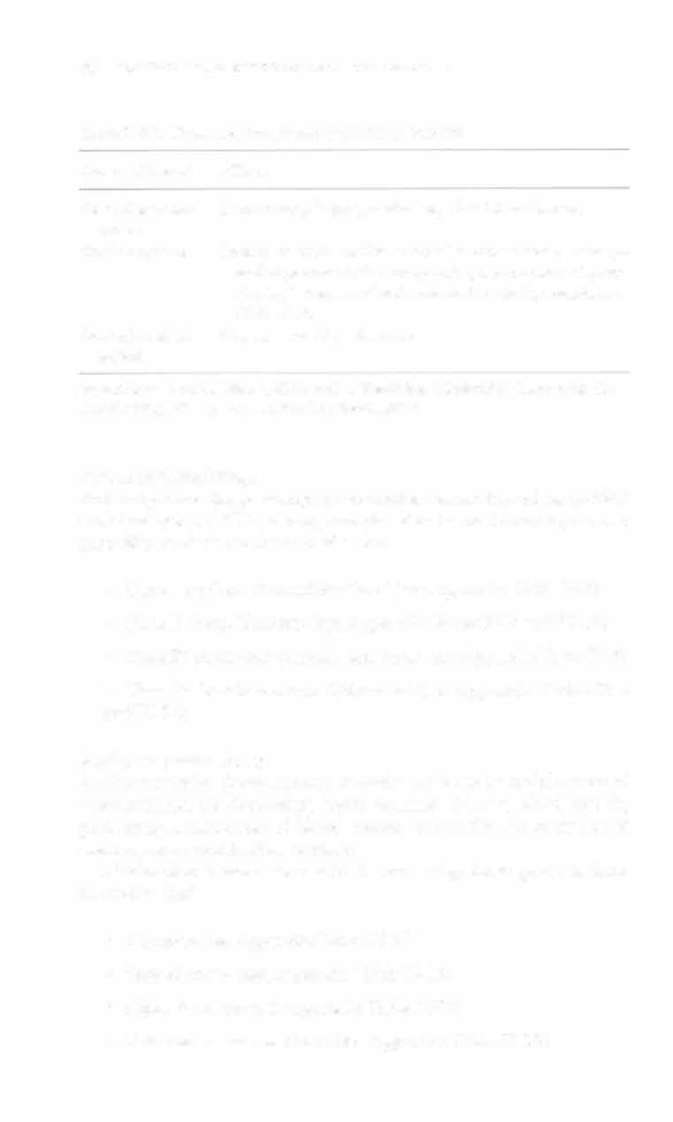
Notc: Digitalis toxicity can occur in patients taking digitalis as a positive inotrope. Refer ro Table 1 -20 for signs and symptoms of digitalis roxicity (digitalis level >2).

60
ACUTE CARE HANDBOOK FOR PHYSICAL THERAPISTS
Table 1-20. Signs and Symptoms of Digitalis Toxicity
System Affecred
Effecrs
Central nervous
Drowsiness, fatigue, confusion, visual disrurbances
system
Cardiac system
Premature atrial and/or ventricular conrracrions, paroxys-
mal supravenrricular tachycardia, ventricular tachycardia, high degrees of atrioventricular block, venrricular
fibrillarion
Gastrointestinal
Nausea, vomiting, diarrhea
system
Source: Data from SL Woods, ES Sivarajian-Froelichcr, S Underhill-Moner (cds). Cardiac Nursing (4th cd). Philadelphia: Lippincott, 2000.
Anriarrhythmic Drugs
Antiarrhythmic drugs attempt to normalize conduction of the cardiac
elecrrical sysrem .'o These drugs are classified in rhe following manner
according to their mechanism of action:
• Class [ (sodium channel blockers) (see Appendix Table IV-3)
• Class II (bera-blockers) (see Appendix Tables IV-3 and IV-l3)
• Class III (refracrory period alterations) (see Appendix Table lV-3)
• Class IV (calcium channel blockers) (see Appendix Tables IV-3
and IV-lA)
Antihypertensive Drugs
Antihypertensive drugs attempt to assist the body in maintenance of
normotension by decreasing blood volume, dilating blood vessels,
preventing constriction of blood vessels, preventing the retention of
sodium, or a combination of these.
Medication classes successful in achieving these goals include
the foliowingSo:
• Diuretics (see Appendix Table IV- I ?)
•
Beta-blockers (see Appendix Table IV- 1 2)
• Alpha-blockers (see Appendix Table lV- 'J 2)
• Calcium channel blockers (see Appendix Table IV- J 4)

CARDIAC SYSTEM
6 1
• AngiOlensin-converting enzyme inhibitors (see Appendix Table lV-2)
• Vasodilators (see Appendix Table lV-30)
Lipid-Lowering Drugs
Lipid-lowering drugs attempt to decrease lipid levels. They are usually
prescribed in combination with a change in diet and exercise habits
(see Appendix Table lV_22).5o Medications successful in lowering
lipid levels are the following:
• Anion exchange resin
• Fibric acid derivatives
• Hepatic 3-methylglutaryl coenzyme A reductase inhibitor
• Nicotinic acid
• Probucol
•
Fish oils
Physical Therapy Intervention
In the acute care setting, physical therapy intervention is indicated for
patients with cardiac impairments that result from CHF, Ml, or status
post CABG. However, a great majority of patients who receive physical
therapy present with one or many other cardiac impairments or diagnoses. Given the high prevalence of cardiac disease in the elderly population and the hospital admissions for the elderly, the likelihood of working with a patient who has cardiac impairment is very high. This
section discusses basic treatment guidelines for physical therapists
working with patients who have present or past cardiac impairments.
Coals
The primary goals in treating patients with primary or secondary cardiac pathology are the following'''
• Assess hemodynamic response in conjunction with medical or surgical management during self-care activities and functional mobility
• Maximize activity tolerance
62
ACtrrE CARE HANDBOOK FOR I'HYSICAL THERAI'ISTS
• Provide patient and family education regarding behavior modification and risk factor reduction (especially in patients with CAD, status post MI, PTCA, CABG, or cardiac transplant).
Basic Concepts for the Treatment of Patiellts
with Cardiac Dysftmcti01t
The patient'S medical or surgical status must be considered in intervention planning, because it is inappropriate to treat an unstable patient.
An unstable patient is a patient who clearly requires medical intervention to stabilize a life-threatening condition. A patient's status may flucruare on a daily or hourly basis. Table 1-2 1 provides general guidelines of when to withhold physical therapy (i.e., instances in which further
medical care should precede physical therapy).5o These are provided as
absolute and relative indications of instability. Relative indications of
instability should be considered on a case-by-case basis.
Once it is determined that a patient is stable at rest, the physical
therapist is able ro proceed with activity or an exercise program, or
both. Figure 1 - 1 0 provides a general guide to determining whether a
patient'S response to activity is stable or unstable.
Everything the physical therapist asks a patient to do is an activity
that requires energy and therefore needs to be supported by the cardiac system. Although an activity can be thought of in terms of absolute energy requirements (i.e., metabolic equivalents-refer to Table 1 - 1 2), an individual's response ro that activity is relative ro that individual's capacity. Therefore, although MET levels can be used to help guide the progression of activity, the physical therapist must be aware
that even the lowest MET levels may represent near-maximal exertion