i bc27f85be50b71b1 (255 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown
814 AClffE CARE HANDBOOK FOR PHYSICAL THERAPISTS
Cuff
Approximately 0.5 in. from the end of an endotracheal or tracheal
tube is a cuff (balloon). The cuff is inflated to (1) ensure rhar all of rhe
supplemenral oxygen being delivered by rhe venrilator via the artificial airway enters the lungs and (2) help hold the artificial airway in place. Cuff inflation pressure should be adequate to ensure that no air
is leaking around the tube; however, cuff pressures should not exceed
20 mm Hg. High cuff pressures have been linked to tracheal damage
and scarring, which can cause tracheal stenosis.
Clinical Tip
• A cuff leak should be suspected if the patienr is able to
phonate or audible sounds come from his or her mouth.
• Cuff leaks can occur if the endotracheal tube is shifted
(positional leak) or if the pressure changes in the cuff.
• If a cuff leak is suspected, then the respiratory therapist
or nurse should be notified. (Physical therapists who specialize in critical or cardiopulmonary care may be able to add air to the cuff according to the facility's guidelines.)
Positive Pressure Ventilators
Positive pressure ventilators are classified based on the method used
to stop the inspiratory phase and allow expiration (cycling method)
to occur.' There are three basic cycling methods: (1) pressure cycled,
(2) volume cycled, and (3) time cycled.
Pressure-cycled ventilators Stop inspiration at a preset pressure,
volume-cycled ventilators stOp inspiration at a preset volume, and
time-cycled ventilators stop inspiration at a preset time interval.
Although these methods allow for increased conrrol of certain variables during inspiration, holding only one variable constant for the termination of positive pressure inhalation allows other factors to
affect inspiration and potentially cause barotrauma or reduced
inspiratory volumes. These factors include position changes and manual techniques.
For example, with a volume-cycled ventilator, a preset volume will
be delivered regardless of the patienr's position, and reductions in
chest wall expansion owing to a patienr's position (e.g., side lying)


APPENDIX 111-8: MECHANICAL VENTILAT10N
815
may increase the pressure placed on the dependent lung tissue and
result in barotrauma. Conversely, in the same scenario, if a patient is
on a pressure-cycled ventilator, then pressure will be delivered to the
predetermined level, but because the patient's position may hinder
chest expansion, a resultant lower volume of inspired air may be
delivered, because the preset pressure limit was reached. Many newer
ventilators provide the clinician with more than one cycling option,
and certain modes of ventilation allow for more than one parameter
ro derermine the inspirarory phase (as discussed throughout this
appendix).
Clinical Tip
• Being aware of the cycling method, the therapist can
pay attention to changes in the pressure or tidal volume
(VT) associated with his or her interventions.
• Wide bore plastic tubing is used to create the mechanical ventilator's circuit. The terminal end of this circuit directly connects ro an endotracheal or tracheal tube or,
less commonly, to a face mask.4 Some ventilator circuits
have an extra parr at their terminal end for an "in-line"
suction catheter, which allows for suctioning without the
removal of the ventilator circuit from the patient.4
Modes of Ventilation
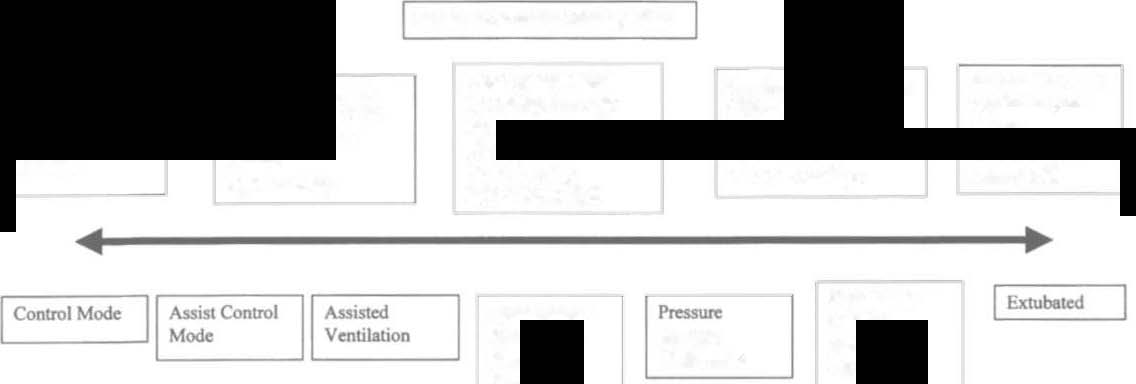
Modes of ventilation can range from providing rotal support (no
work performed by the patient) to minimal support (near-total
work performed by the patient). Modes of ventilation are geared
toward allowing the patient to do as much of the work of breathing as is physiologically possible, while meeting the intended objectives of ventilatory support. Even short periods (11 days) of
complete dependence on positive pressure ventilation can lead to
respiratory muscle atrophy and concomitant reductions in diaphragm strength (25%) and endurance (36%).5 Figure III-B.2 provides a schematic of the conventional modes of ventilation based on the amount of support they provide. Characteristics of conventional and alternative modes of ventilation are presented in Tables III-B. I and III-B.2, respectively.

00
�
Sp«trum ofPatienl Participation
'"
,.
No
Good Spontaneous
lndependent with
Spontaneous
Some Spontnneous
Spontaneous Breathing:
Brearbing: RR> 10
�
ventilation and
Breathing
(RR < 10)
-
Breathing: RR < 10
Total
But inspiratory effort
able to
Ventilator
Weak. inspiratory
Good EfTon:
9
still weak:
physiologically
Dependence
effons:
VT> 10 m.Vkg
i:;
Vt < 10 mllkg
support self
VT<6mL1kg
NIF> 20 em H:O
NlF < 10 em H10
s;
�
�
o
"
Continuous
Synchronous
lntenni
Positive
�
ttem
Support
Airway
Mandatory
Ventilation
p..,....
OJ!
Ventilation
�
§
,..
Figure ill-B.2. Schematic of mechanical ventilator modes: the ability of patients to participate in the process of ventilation and i
oxygenation in part determines the mode of ventilation. Parameters used to determine the patient's ventilatory effort include the iii
presence of spontaneous breaths, the number of breaths per minute he or she initiates (respiratory rate [RR)). the volume of
>-
'"
those breaths per breath (tidal volume /VT}). and the negative inspiratory force (NIF) generated with those breaths. The values B
indicated above are examples 0/ patient characteristics along the spectrum (rom complete ventilatory dependence to independence. The effectiveness of the patient's efforts needs to be assessed based not only 011 the above parameters. but on "outcon-te"
variables, such as oxygenation (Pao'}! oxygen saturation as measured by pulse oximetry). ventilation (Paco2), and overall status (hemodynamic stability. symptonts).

APPENDIX III-B: MECHANICAL VENTILATION
817
Table HI-B.l. Conventional Modes of Ventilation
Modes
Characteristics
CV
Toral control of the parient's ventilation: preset rate; Fiol; VT;
flow rate; I:E ratio.
Patients may be sedated or pharmacologically paralyzed.
No active respirarory muscle activity is necessary.
AV
Patient controls cespirarory parrern and rare; breath initiated
by patient creares negative airway pressure in circuit; once
initiated, the volume is delivered with eirher a preset
volume or pressure and flow ratc; respiratory muscles are
still working.
Patient can trigger RRs that are roo high, leading ro
respirarory alkalosis or auto PEEP (see text).
A ssist!
Combination of CV and AV; delivers breath of predetermined
control
tidal volume with the patient'S inspiratory effort.
ventilation
If the patient does not initiate a breath within a specified time
period, the ventilator will deliver a breath ro maintain
preset RR.
IMV
Delivers breaths intermittently at preset time intervals with a
preset RR, VT,and flow rare.