i bc27f85be50b71b1 (253 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown

Table lU-A.6. Continued
00
�
Device
Description
Clinical Implications
>
• Yankauer suctioning may stimulate a
�
cough and help clear secretions in
�
patients who are unable to dear
i:i
secretions independendy.
J:
�
• If a patient bites down on the
o
Yankauer, do not anempt to pull on
�
o
the device. Wait for the patiem to
'"
relax, then gendy slide the Yankauer
o
;0
from the patiem's mouth.
i:
AV
�
= arteriovenous; CSF = cerebrospinal fluid; CVP = central venous pressure; TPN = total parenteral nutrition.
i'i
>
• Listed in alphabetical order.
...
Sources; Data from RR Kirby, RW Taylor, JM Civena (cds). Handbook of Critical Care (2nd cd). Philadelphia: Lippincorr-Raven, 1 997; F Hal
:;I
derman. Selecting a vascular access device. Nursing 2000; 1 1 :59-61; DF Colixxa. Actionstat: dislodged chest rube. Nursing 1 995;25-33; I-IJ
m
Thompson. Managing patients with lumbar drainage devices. Crit Care Nurse 2000;20:60-68; and Guidelines for intensive care unit admission,
�
discharge, and triage. Task Force of the American College of Critical Care Medicine, Society of Critical Care Medicine. Crit Care Med 1999;27:
�
633--638.

APPENDIX III-A: MEDICAL-SURGICAL EQUIPMENT IN 11-IE ACllfE CARE SETTING
807
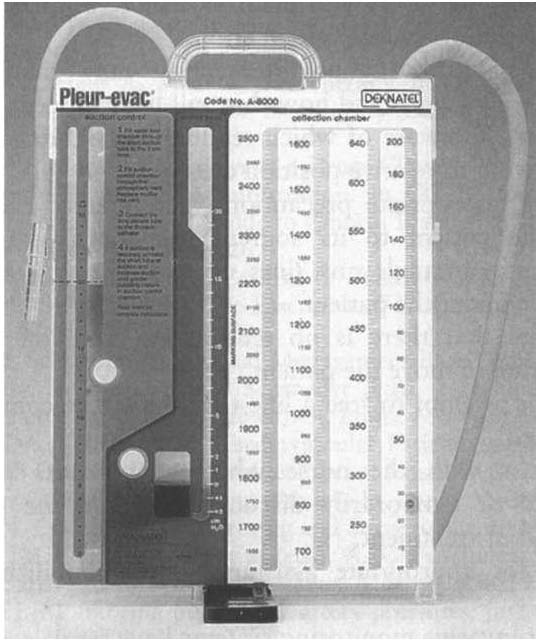
Figure [[I-A. I O. A chest drainage system has three mai" compartments from
left to right: (1) the suction control. (2) the water seal. (3) the collection
chamber. (Reprinted with permission from Genzyme Biosurgery.)
place (e.g., conract precautions) . Refer to Table 10-4 for a
summary of infection prevention precautions.
•
Practice universal precautions. The likelihood of
encountering bodily fluids is increased in the aCllte care
serring, especially in rhe ICU.
•
Discuss your planned intervention with the nurse.
Scheduled procedures may rake precedence over rhis intervention, or it may coordinate well with another planned
procedure.
•
On entering the patient's room, take inventory. Observe
rhe parient's appearance and posirion. Systemarically
observe rhe parient and verify rhe presence of all documenred lines. Develop a consistent method of surveying rhe room: lefr to righr, or rop of bed ro bottom of bed, ro
ensure rhar all lines and equipmenr are observed and con-


808 ACUTI CARE HANDBOOK FOR PHYSICAL THERAPISTS
side red in your treatment plan. Take note of all readings
on the monitors before intervention.
•
Anticipate how your intervention may change the
patient's vital signs and how this will likely appear on the
monitors. Be aware of which readings may change artificially owing to relative position change.
•
Using appropriate precautions, gently trace each line
from the patient to its source. Ask for assistance, if
needed, to untangle any lines or to free any lines that
might be under the patient.
•
Ensure that there is no tension on each line before
attempting to move the patient.
•
Never arrempt to free a line that cannot be completely
visualized!
•
Discuss with the nurse whether any lines can be
removed or temporarily disconnected from the patient
before your treatment.
•
Ask for appropriate assistance when mobilizing the
patient.
•
Most invasive monitoring systems have two alarm controls: one to silence or discontinue the alarm for a few
minutes, and another to disable or turn off the alarm. Do
not silence or disable an alarm without permission from
the nurse!
•
On completion of your tteatment, ensure that all appropriate alarms are turned on and that the patient is positioned with the appropriate safety and communication measures in place. Notify the nurse of any change in the
patient'S status.
References
1 . Anonymous. Guidelines for intensive care unit admissions, discharge, and
triage. Task Force of the American College of Critical Care Medicine,
Society of Critical Care Medicine. Crit are Med 1 999;27(3),633--j)38.
2. Kirby RR, Taylor RW. Oxygen Therapy. In RR Kirby, RW Taylor, JM
Civetta (cds), Handbook of Critical Care (2nd cd). I'hiladelphi., Lippincon-Raven, 1 997;254,260.