i bc27f85be50b71b1 (85 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown

284
ActrrE CARE HANDBOOK FOR PHYSICAL THERAPISTS
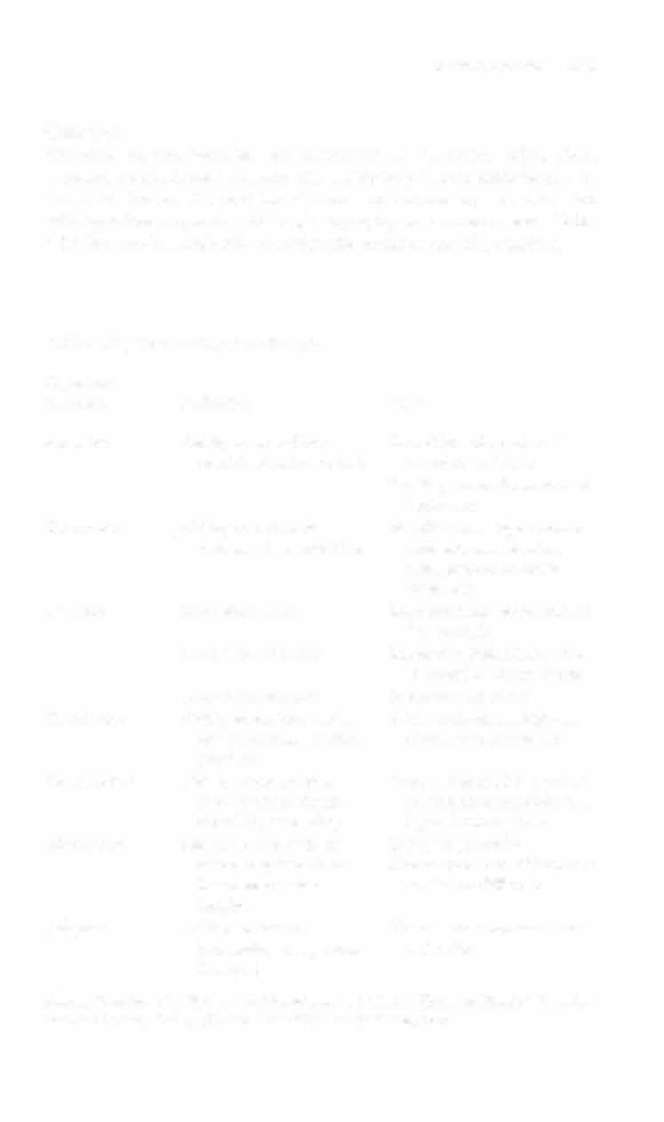
Table 4-11. The Glasgow Coma Scale
Response
Score
Eye opening (E)
Spontaneous: eyes open without stimulation
4
To speech: eyes open to voice
3
To pain: eyes open to noxious stimulus
2
Nil: eyes do nor open despite variery of stimuli
Motor response (M)
Obeys: follows commands
6
Localizes: purposeful anemprs to move limb to sdmuJus
5
Withdraws: flexor withdrawal without localizing
4
Abnormal flexion: decorticate posturing to stimulus
3
Extensor response: decerebrate posturing [Q stimulus
2
Nil: no motor movement
Verbal response (V)
Oriented: normal conversation
5
Confused conversation: vocalizes in sentences, incorrect
4
context
Inappropriate words: vocalizes with comprehensible
3
words
Incomprehensible words: vocalizes with sounds
2
Nil: no vocalization
Source: Data from B jennen, G Teasdale (cds). Management of Head Injuries. Phibdel·
phia: FA Davis, 198 I .
score (i.e., E + M + V). Scores range from 3 to 15. A score of 8 or less
signifies coma.10
Clinical Tip
Calculation of the GCS usually occurs at regular intervals.
The GCS should be used to confirm the type and amount
of cueing needed to communicate with a patient, determine what time of day a patient is most capable of participating in physical therapy, and delineate physical therapy goals.

NERVOUS SYSTEM
285
Cognition
Cognitive testing includes the assessment of attention, orientation,
memory, abstract thought, and the ability to perform calculations or
conStruct figures. General intelligence and vocabulary are estimated
with questions regarding history, geography, or current events. Table
4- 1 2 lists typical methods of testing the components of cognition.
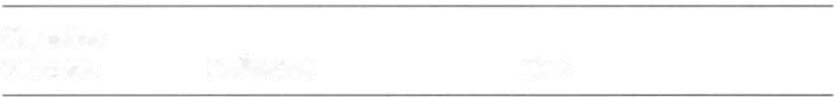
Table 4-12. Tests of Cognitive Function
Cognitive
Function
Definition
Task
Attention
Ability to artend to a
Repetition of a series of
specific stimulus or task
numbers or lerrers
Spelling words forward and
backward
Orientation
Ability to orient to
Identify name, age, current
person, place, and time
date and season, birth
date, present location,
rown, etc.
Memory
Immediate recall
Recount three words after a
few seconds
Short-term memory
Recount words (after a few
minutes) or recent events
Long-term memory
Recount past events
Calculation
Ability to perform verbal
Add, subtract, multiply, or
or written mathematical
divide whole numbers
problems
Construction
Ability to construct a
Draw a figure after a verbal
two- or three-dimencommand or reproduce a
sional figure or shape
figure from a picture
Abstraction
Ability to reason in an
Inrerpret proverbs
abstract rather than a
Discuss how two objects are
literal or concrete
similar or different
fashion
Judgment
Ability to reason
Demonstrate common sense
(according to age and
and safery
lifestyle)
Source: Dam from LS Bickley, RA Hoekelman (cds). 8ate's Guide fO Physical Examination and History Taking {7th cd}. Philadelphia: Lippincott, 1999.
286
ACtITE CARE HANDBOOK fOR PHYSICAL THERAPISTS
Emotional State
Emotional State assessment entails observation and direct questioning to ascertain a patient's mood, affect, perception, and thought process, as well as to evaluate for behavioral changes. Evaluation of
emotion is not meant to be a full psychiatric examination; however,
it provides insight as to how a patient may complete the cognitive
portions of the mental status examination. I I
Clinical Tip
It is important to note that a patient's culture may affect
particular emotional responses.
Speech and Language Ability
The physician should perform a speech and language assessment
as soon as possible according to the patient'S level of consciousness. The main goals of this assessment are to evaluate the patient'S ability to articulate and produce voice and the presence,
extent, and severity of aphasia." These goals are achieved by testing comprehension and repetition of spoken speech, naming, quality and quantity of conversational speech, and reading and writing abilities. 12
A speech-language pathologist is often consulted to perform a
longer, more in-depth examination of cognition, speech, and swallow using standardized tests and skilled evaluation of articulation, phonation, hearing, and orofacial muscle strength testing.
Clinical Tip
• The physical therapist should be aware of and use, as
appropriate, the speech-language pathologist's suggestions
for types of commands, activity modification, and positioning as related to risk of aspiration.
• The physical therapist is often the first clinician to
notice the presence or extent of speech or language dysfunction during activity, especially during higher-level tasks or those activities that cause fatigue. The physical
therapist should report these findings to other members of
the health care team.


NERVOUS SYSTEM
287
Vital Sig1ts
The brain is the homeostatic center of the body; therefore, vital
signs are an indirect measure of neurologic status and the body's