Pediatric Primary Care (14 page)
B. Milk collection and storage.
1. Recommendations for collection and storage of mother's milk for hospitalized infant differ from that of the following instructions for the well child at home.
2. Mothers should wash hands thoroughly prior to pumping.
3. Follow manufacturer's instructions for cleaning of pump parts.
4. Glass containers with lids are a good choice for storing milk. Hard plastic (polypropylene) can also be used. Avoid bottles made with bisphenol A.
5. Mother can encourage milk let down by looking at picture of baby, smelling piece of baby's clothing.
6. Warm, wet washcloths on breast combined with breast massage may be helpful in starting milk flow.
7. Breastfeeding on one breast while pumping from other breast is an option.
8. All pumps are different. Encourage mother to find one that creates comfortable seal, which provides appropriate suction. Pumping should not be painful.
9. For specific information on storing milk for home use for full-term infants see the Academy of Breastfeeding Medicine Revised Protocol #8 March 2010.
IX. SUPPORTING BREASTFEEDING PAST THE EARLY DAYS
A. Follow up.
1. Breastfeeding infants should be evaluated by an appropriate healthcare professional at 3-5 days of age and again at 2-3 weeks for successful feeding and appropriate weight gain. Infants should always be evaluated in between scheduled visits for any concerns.
2. Breastfeeding mothers should be referred to a breastfeeding support group following hospital discharge.
B. Maternal diet.
1. Encourage mother to eat a wide variety of healthy foods, eating when hungry, drinking to quench her thirst.
a. Forcing large quantities of fluids will not increase her milk production.
b. No specific foods must be avoided by breastfeeding mothers.
c. Most foods do not bother most babies.
d. If particular food seems to bother baby, decrease/eliminate for a week to 10 days.
2. It is recommended that all breastfed babies be supplemented with vitamin D 400 IU starting soon after birth.
3. Families with significant allergies should receive knowledgeable dietary counseling regarding possible need to eliminate certain foods while breastfeeding.
C. Growth spurts.
1. Regardless of culture, women frequently worry about ability to provide enough milk for baby.
2. Teach parents that growth spurts (periods when babies want to nurse more frequently to meet rapid growth) usually occur around 2-3 weeks, 6 weeks, 3 months.
3. Feed as often as baby wants to nurse to increase, then maintain adequate milk supply.
4. Reinforce concept of supply and demand.
5. Supplementing with formula is strongly discouraged; mother's milk supply will not increase without adequate stimulation to meet baby's growing demand for more milk.
D. Medications and breastfeeding.
1. It is imperative that healthcare providers give information to mothers who breastfeed on the safety of medications based on appropriate, current research, citing the source. Each infant's individual situation must be assessed prior to determining the appropriate use of any medication during breastfeeding. An excellent reference guide such as Hale (2010) should be available in every clinical setting that deals with breastfeeding mothers. Drugs listed are assigned a lactation risk category from L1 (safest) to L5 (contraindicated).
2. Many of the medications likely to be prescribed to breastfeeding mothers should not affect maternal milk supply or infant's safety. Ibuprofen is a commonly used analgesic postpartum and is considered compatible with breastfeeding. Penicillins and cephalosporins, along with several of the selective serotonin reuptake inhibitors (SSRIs) often used for depression, are also generally considered compatible.
3. Dose of medication transferred through breastmilk is almost always too low to be clinically significant or it is poorly bioavailable to infant.
4. It is preferable for mothers to avoid using medication whenever possible.
5. Extensive benefits of breastfeeding far outweigh any potential risks in majority of cases.
a. Medications should be safe for infants to consume.
b. Choose drugs with breastfeeding information whenever possible.
c. Choose shortest acting form of medication.
d. Encourage feeding when maternal drug level is lowest.
e. Educate parents as to potential side effects to observe in infant, and affect on milk supply.
f. Be extra cautious with preterm, low birth-weight or sick infants.
g. Certain herbal substances may be harmful to infants.
h. Drugs of abuse are contraindicated in breastfeeding and temporary cessation of breastfeeding is necessary with certain radioactive compounds, and a few medications. Consult appropriate resources for detailed information.
E. Maternal employment.
1. Women who return to work must be well supported in effort to continue providing breastmilk for infant.
2. Women need a private, clean place to pump every few hours while separated from infant.
3. Expressed milk can be kept at room temperature for short periods, in insulated bag with cooler pack, or, if available, in refrigerator. Encourage mothers to rent or purchase pump that is comfortable and is efficient for their particular needs.
4. Provide information on how to introduce bottle to the infant, as well as suggestions for caregiver that will promote extended breastfeeding (i.e., not bottle feeding immediately before mother will pick up infant, proper handling, storage of breastmilk).
5. Returning to workplace while continuing to provide breastmilk for baby may initially seem overwhelming to some mothers. Strong encouragement, praise, support can make difference between mother being successful and giving up.
6. Some employers are now required to provide break time for nursing mothers under the Patient Protection and Affordable Care Act, signed in to law on March 23, 2010.
X. COMMON PROBLEMS
A. Mothers can complain about pain even when damage is not visible on the breast or nipple. Determine that baby is positioned properly at breast height with adequate support and is latching on correctly. Mothers often describe sensation of baby feeding as strong tugging sensation. Breastfeeding should not be painful. Nipples do not “toughen up” as breastfeeding proceeds. Assess for other causes of sore nipples such as trauma, improper latch and release, thrush, milk plugs on nipple, incorrect use of breastfeeding devices or tight frenulum (see
Figure 5-8
).
Paget's disease, an uncommon type of breast cancer, must also be ruled out. Breastfeeding issues that do not resolve quickly should promptly be referred to pediatric or maternal experts for further management.
B. Sore nipples management includes:
1. Correct positioning and latch-on.
2. Teach mothers to express colostrum/hindmilk to apply to nipples after each feeding.
3. Allow nipples to dry before putting bra back on.
4. Offer use of breast shells to prevent fabric from rubbing against sore nipples.
5. Breastfeed from least sore side first.
6. Change positions at each feeding to decrease pressure on sore area.
Figure 5-8
Tight frenulum.
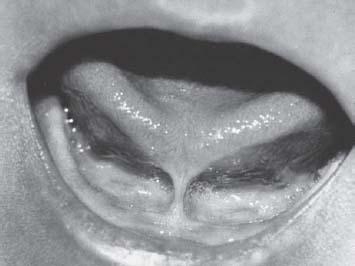
Source:
Riordan J, Wambach K.
Breastfeeding and Human Lactation.
4th ed. Sudbury, MA: Jones & Bartlett Learning; 2010.
7. Suggest moist wound healing methods (i.e., modified lanolin or hydrogel dressings).
8. Analgesics as needed.
C. Flat or inverted nipples.
1. Can initially make breastfeeding more of a challenge, may be difficult for baby to latch on, suck well. Provide adequate support to ensure successful feedings.
2. ”Pinch test”: determines if nipple is flat or inverted upon compression. With thumb behind nipple and first two fingers underneath, grasp about 1 in. back from base of nipple and compress skin.
a. Normal nipple will evert.
b. Flat nipple remains flat with compression.
c. Inverted nipple looks sunken in.
d. Nipples can look flat or inverted, but evert on compression.
3. Flat or inverted management includes:
a. Encouraging deepest possible latch onto breast.
b. Making sure infant is at breast height and well supported to prevent sliding to base of nipple.
Other books
Hannah Howell by Highland Hearts
Laure Donavan 2 - Ghouls Night Out by Rose Pressey
Every Time We Kiss by Christie Kelley
Where Your Heart Is (Lilac Bay Book 1) by Rachel Schurig
Nutshell by Ian McEwan
(Never) Again by Theresa Paolo
The Heat is On by Elle Kennedy
Sally Berneathy - Death by Chocolate 03 - The Great Chocolate Scam by Sally Berneathy
Fleeting Moments by Bella Jewel