Pediatric Primary Care (15 page)
c. Release latch and repeat attempts until proper latch is obtained. Allowing baby to suck at base of nipple prevents stimulating milk supply, will cause sore nipples.
d. Encourage offering flat/inverted breast first when baby is hungriest and sucking is strongest.
e. Teach mother to evert nipple with gentle pulling/rolling immediately prior to latch.
f. Hand express few drops of colostrum to entice baby to latch on.
g. Use hand/electric pump for few minutes immediately prior to latch.
h. If supplement is medically indicated, use expressed milk first using an eyedropper, syringe, cup, or feeding tube at the breast.
i. Avoid pacifiers and bottle nipples until breastfeeding is well established.
D. Severe engorgement.
1. Milk stasis caused by inefficient, infrequent removal of milk, results in extremely full, swollen, lumpy, painful breasts.
2. Result is different from transient breast fullness associated with milk “coming in” 2-4 days after birth.
3. Breastfeeding emergency: milk stasis can cause damage to tissue, decrease milk supply, and make it difficult to impossible for infant to compress areola and remove milk.
4. Severe engorgement management includes:
a. Analgesics as necessary.
b. Warm, wet compresses to breast prior to feedings to help increase milk flow.
c. Soften areola using hand expression so baby can latch properly.
d. Use breast compression during feedings to improve milk flow. Using her thumb on top of breast and her fingers underneath, the mother brings her fingers together, which compresses breast.
e. Use of cold compresses may help to decrease engorgement after feeding. Some mothers like to use this prior to feeding as well.
f. Use of chilled green cabbage leaves left on breast for short period several times/day can be helpful to some mothers. Stop using this as soon as engorgement decreases.
g. Express milk after feeding as needed for comfort. Any expressed milk can be fed to baby using alternative feeding methods.
E. Mastitis.
1. Infection of breast, usually caused by
Staphylococcus aureus.
2. Frequently occurs in upper outer quadrant of breast, often by 2-3 weeks postpartum.
3. Symptoms commonly include hard, swollen, reddened area on breast accompanied by flu-like symptoms.
4. Difficult to differentiate between engorgement, plugged duct, mastitis
(
Table 5-1
).
5. Mastitis management includes:
a. Rest (decrease stress and fatigue by enlisting support from friends, family).
b. Antibiotics; encourage completing full course as prescribed.
c. Increase maternal fluid intake.
d. Frequent, effective emptying of breasts (important to continue breastfeeding, milk is not infected, fine for baby).
e. Abrupt weaning can predispose to an abscess.
f. Analgesics as needed.
g. Correct latch to prevent further nipple trauma (cracked, bleeding nipples allow bacteria to enter milk ducts).
h. Mother's preference of warm or cool packs for comfort.
Table 5-1
Comparison of Findings of Engorgement, Plugged Duct, and Mastitis
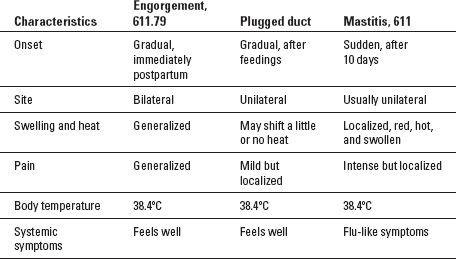
Source:
Lawrence RA, Lawrence RM.
Breastfeeding: A Guide for the Medical Profession.
6th ed. St Louis: Mosby; 2005.
F. Jaundice.
1. Rarely requires cessation of breastfeeding.
2. Pathologic jaundice, with onset in first 24 hours of life, warrants medical evaluation in addition to lactation support.
3. Encourage early initiation of breastfeeding, then frequent, effective, unrestricted feedings to minimize jaundice.
4. Colostrum acts as laxative, eliminating bilirubin through meconium expulsion.
5. Physiologic jaundice, which begins 48-72 hours after birth and peaks on day 3-5, is seen in thriving infants with normal weight gain and output.
6. Observe for effective breastfeeding and continue assessment for normal weight gain and output. Onset and peak of breastfeeding associated with jaundice is similar to physiologic jaundice, but infant is fussy/sleepy with poor feeding and inadequate weight gain, output.
7. Assist with frequent, unrestricted, effective breastfeeding.
8. Teach parents to watch for signs of milk transfer during feedings. If necessary, express milk in addition to feedings, use alternate feeding methods to give baby milk.
G. Thrush.
1. Often described as burning, itching, stinging lasting throughout feeding and beyond, radiating from nipple and breast to shoulder and back.
2. Nipple or areolar skin is often red and shiny.
3. May have period of pain-free nursing, then have sudden onset of pain.
4. Pain from poor latch is often described as feeling like a knife or being stabbed, dissipates as feeding progresses, frequently limited to nipple and areola.
5. Regardless of nipple pain, poor latch must be corrected immediately.
6. Broken skin is perfect environment for organisms to invade.
7. Signs in infant may range from nothing to white patches on buccal mucosa, tongue, and palate, which may bleed when scraped with tongue blade. Fiery red diaper rash with shiny red patches and pustules may also be present.
8. Both mother and baby should be treated simultaneously with appropriate antifungal medications to prevent reinfection from one to the other.
9. All objects (pumping supplies, pacifiers, bottles) coming in contact with baby's mouth should be boiled daily.
10. Mothers should be encouraged to continue breastfeeding while treating infection.
11.
Candida albicans
thrives in warm, moist, dark areas. Nipples can be rinsed with clear water or vinegar solution of 1 tablespoon vinegar in 1 cup of water after each feeding, exposing to air after each feeding.
12. Bed linens, sheets, bras can be rinsed in vinegar solution after hot wash cycle. Breast pads should be disposable and changed as soon as wet.
13. Sexual contact between mother and partner can spread infection. Partner should be treated appropriately.
H. Weight gain concerns.
1. Breastfed infants gaining less than appropriate amount for age should be carefully evaluated. Often, correcting latch and positioning is enough to facilitate efficient breastfeeding and improve weight gain.
2. Do not recommend formula supplementation without evaluating breastfeeding. If extra calories are needed, have mother hand express or pump in addition to breastfeeding and use alternative feeding methods to give baby milk.
3. Allowing baby to finish feeding on one breast before feeding on second allows sufficient amounts of higher calorie breastmilk.
4. Review with parents appropriate signs of infant hunger, encourage frequent (8-12 or more/24 hours) unrestricted feedings.
5. Keeping written log of feedings and output is also helpful. Imperative that infant have adequate caloric intake.
6. If after evaluation and management with skilled breastfeeding consultant, breastfeeding is not going well, formula supplementation is appropriate. Plan for maintaining/increasing mother's milk supply must be implemented.
7. Return office visit within 24-48 hours to monitor situation should be scheduled. Frequent phone follow up, support are necessary.
8. Global growth charts released by the World Health Organization (WHO) in 2006 reflect standards on how children should grow based on breastfeeding as the norm.
XI. HELPFUL BREASTFEEDING RESOURCES
A. Locating a board-certified lactation consultant:
International Lactation Consultant Association
919-861-5577
www.ilca.org
International Board of Lactation Consultant Examiners
703-560-7330
www.iblce.org
Breastfeeding National Network (BNN)
1-800-TELL-YOU
www.medela.com
Other books
Johnny Cash: The Life by Hilburn, Robert
Louise Rennison_Georgia Nicolson 04 by Dancing in My Nuddy Pants
Exclusive by Fern Michaels
Colony Z: The Complete Collection (Vols. 1-4) by Luke Shephard
Under a Summer Sky by Nan Rossiter
At Empire's Edge by William C. Dietz
East End Trouble by Dani Oakley, D.S. Butler
Blood Work by Mark Pearson