This is Living (Living #1.5)
Read This is Living (Living #1.5) Online
Authors: Melody Dawn
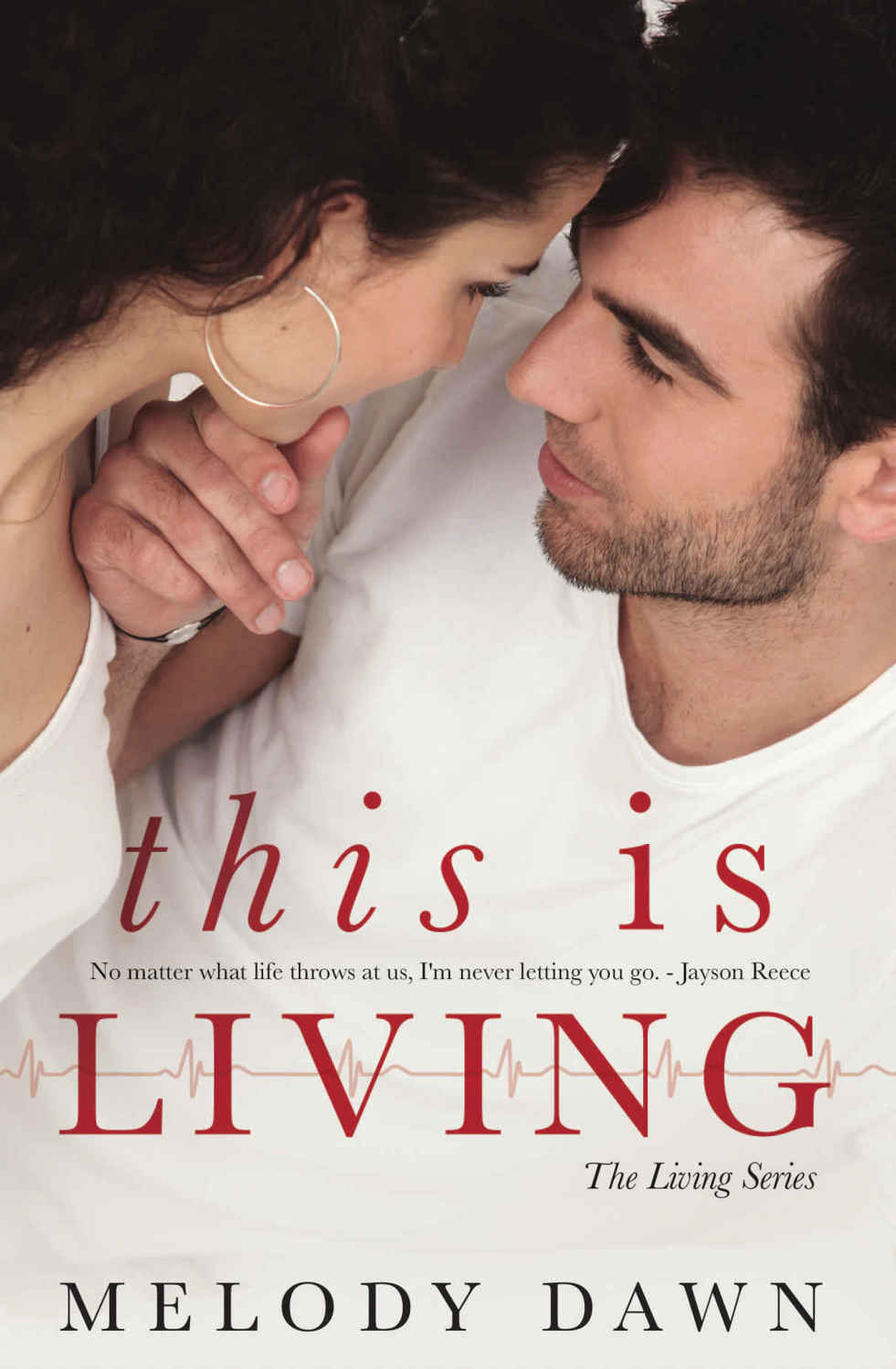
This is Living
Copyright © 2016 Melody Dawn
All rights reserved. No part of this book may be reproduced or transmitted in any form, including electronic or mechanical, without written permission from the publisher, except in the case of brief quotations embodied in critical articles or reviews.
This is a work of fiction. Names, characters, businesses, places, events, and incidents are either the products of the author’s imagination or used in a fictitious manner. Any resemblance to actual persons, living or dead, or actual events is purely coincidental.
This book is licensed for your personal enjoyment only. This book may not be re-sold or given away to other people.
If you would like to share this book with another person, please purchase an additional copy for each recipient. If you are reading this book and did not purchase it, or it was not purchased for your use only, then please return to your favorite eBook retailer and purchase your own copy. Thank you for respecting the hard work of this author.

Table of Contents

Another book…another dream realized
Marisa-Rose Shor with Cover Me, Darling
Samantha Wiley with Proofreading By the Page
Brenda Wright with Formatting Done Wright
Maria Lazarou with Obsessive Pimpettes
Melody’s Hot Chicks
To my beta readers: Thanks so much for your help
To Judy: I love our late night chats…can’t wait for more
To Jenna: because you make me laug
h
To RJ Thompson aka Jenn: your work inspires me greatly and I’m so proud to call you my friend.
To Crystal: the best friend a girl could have and we share a brain so I kind of have to love you lol ;)
To my husband: I love you more than life
To God: because you’re always there for me.
To my 5 angel babies: you are forever in my heart
With love,
Melody Dawn

 Present Day
Present DayI’ve been here for over 18 hours and though my shift is actually over, I’m unable to leave due to the massive patient load. There’s no way only one doctor could handle this alone and still treat on a proficient level.
A wave of exhaustion rolls over me and I wish I could start a caffeine IV to drive away my tiredness. Instead, I grab a cup of coffee from the ER community coffee pot and drink as fast as I can without burning my mouth irreparably. Although it tastes like shit, I need it to help me keep going. I don’t have the luxury of giving into my lack of sleep, especially when I’m treating cases such as the one on its way in.
A crew from Acadian Ambulance called in to report a few moments ago that they will be arriving with a barely responsive 46 year old male exhibiting signs of cardiac distress. The EKG forwarded from the ambulance shows definitive abnormalities that will have to be treated right away.
The ER radio crackles and a voice announces their impending arrival with the critical patient. The nurses have already set up a room with everything we might need to treat him so now there’s nothing left to do but wait.
LaTasha, my charge nurse for the evening, alerts me to the patient’s arrival.
“Dr. Reece, your cardiac case is coming in.”
Just as she finishes her sentence, the ambulance entrance to the ER slides open and two medics rush in with my newest patient. He is pale and showing signs of shortness of breath even though he has a nasal cannula of 100% O2 going.
“Room 2,” I bark at everyone following me.
Pushing him into the assigned room, the paramedics go about transferring him to our gurney while the nurses check his vitals.
“Mr. Santiago, I’m Dr. Reece. Can you tell me where your pain is located and on a scale of 1-10, how bad you’re hurting?”
I see him trying to make sense of my words and one of the guys that brought him in says, “He only speaks Spanish.”
Immediately, I switch over to Spanish to make him more comfortable. I introduce myself and ask where his pain is located as well as the intensity of it.
“Senor Santiago, soy el Dr. Reece
.
¿
Me puede decir donde se encuentra el dolor y en una escala de 1-10, lo mal que te haces da
ñ
o?”
Looking relieved that he can understand me, he points to mid-sternum and motions down his right arm.
LaTasha brings over his newest EKG strip and comparing it to the original, I see his heart rhythm is deteriorating.
“Page Dr. Najalani for a cardiac consult and do a blood draw for a CBC, chem 12, and cardiac enzymes. Also, hang a bag of 5% dextrose with a bolus of Amiodarone. Repeat his EKG and if there’s no improvement, come and get me. Let me know when Dr. Najalani gets here.”
Knowing that she will follow my instructions to the letter, I make my way back over to the patient’s bed to see what else he might need to make him as comfortable as posible.
Continuing in Spanish, I ask if he needs anything for pain and what number he is rating his discomfort.
He grimaces and replies that he puts it at 20. Since our pain scale is only 1-10 and all of his symptoms point towards a heart attack, I can see why he felt the need to give me an overly high number.
I look over at LaTasha, “He says his pain is at a 20. Give him 4mg of Morphine, IV push, but keep a close check on his blood pressure and heart rate. I don’t want his BP to bottom out from the meds. If he doesn’t get any relief, let me know. I’ve got to see some other patients. Come find me if anything changes. Otherwise, I’ll be checking in as often as I can.”
Switching back to Spanish, I try to reassure him, “Mr. Santiago, I will be checking on you and LaTasha will be taking care of you as well. I’ve also called in one of our best cardiologists to take a look at you.
He reaches up and grabs my had, “Gracias, doctor.”
Thank you, doctor.
A feeling of warmth goes through me and that’s exactly why I didn’t become an engineer. It’s times like this when my career decision makes the most sense…I want to give people hope when they’re at their lowest.
Now it’s a waiting game to see the results of his blood tests and how he responds to the medication… unless his condition goes south…then we’ve got a huge problem.
I make my way back to the ER desk and chart his progress before moving on to my next batch of patients. Vaguely, I notice it’s getting close to my sons’ bedtime and time for my nightly phone call. I make a mental note to take a short break after my next few cases.
Unfortunately, that never happens. Instead, I spend the next few hours bogged down with patients. By the time, I’m able to take a break, I fall into one of the beds in the doctor’s lounge and my phone call is forgotten.
