Read Examination Medicine: A Guide to Physician Training Online
Authors: Nicholas J. Talley,Simon O’connor
Tags: #Medical, #Internal Medicine, #Diagnosis
Examination Medicine: A Guide to Physician Training (20 page)
FIGURE 5.19
(a) PA chest X-ray showing implanted cardioverter defibrillator and biventricular pacemaker. (b) Lateral view: the large defibrillation electrode (which also serves as an RV pacing electrode) (arrow) and the right atrial and left ventricular pacing leads are visible. Figures reproduced courtesy of The Canberra Hospital.
•
The periprocedural mortality rate is less than 1%, compared with over 5% when surgical implantation was required.
The programming of these machines is complicated, but candidates should know that they are usually set to attempt reversion of VT by overdrive pacing (antitachycardia pacing, ATP) before administering a DC shock. Patients are usually, but not always, aware of the onset of ATP and almost always aware of DC shock administration. Ask how the device has affected the patient’s life and confidence, including how often it goes off and whether the box itself causes problems because of its size. Although AICDs can prevent sudden death, their presence is often associated with a feeling of insecurity. Patients may have clear memories of events leading up to activation of the device. They may avoid places where arrhythmias and activations have occurred. They often require repeated explanation and reassurance.
The particular management problems of atrial fibrillation
Examiners require candidates to have a sensible approach to the management of AF and the opportunity for examiners to ask about this common condition will often arise. The principles of management are to:
•
maintain sinus rhythm
•
control the heart rate (if maintaining sinus rhythm proves difficult)
•
protect from embolic events.
1.
There is good evidence from recent trials that control of heart rate is at least as satisfactory an approach as that of trying aggressively to maintain sinus rhythm. Nevertheless, patients with paroxysmal AF often find the arrhythmia very disturbing. They should be told at the outset that it may not be possible to keep them in sinus rhythm, but that rate control and freedom from embolic episodes can be achieved. The prophylactic drug treatment of paroxysmal AF involves the use of a class III drug (sotalol or amiodarone) in most cases, but occasionally the class 1C drug flecainide can be used if the heart is known to be structurally normal.
2.
Rate control of persistent or paroxysmal AF can be achieved with less-toxic drugs. Digoxin is a common first-line treatment and is usually well tolerated. It is not very effective on its own at controlling the heart rate during exercise. Many patients with chronic AF have persistent dyspnoea during exercise because of inadequate rate control. They benefit from the use of a beta-blocker or one of the non-dihydropyridine calcium channel blockers (diltiazem or verapamil). These can be used with or without digoxin. Control of the heart rate can prevent or reverse the impairment of left ventricular function that is associated with tachycardias (tachycardia-induced cardiomyopathy).
3.
When patients remain unhappy with their symptoms despite rate control, further intervention should be considered. AV nodal ablation is a relatively simple procedure that prevents fibrillation waves from reaching the ventricles. The patient then requires an artificial pacemaker. Although atrial systole is lost, the regularisation of the heart rate is usually enough to dramatically improve symptoms. If the patient’s AF has been paroxysmal, a dual-chamber pacemaker with a ‘mode switch’ may be used. When the patient is in sinus rhythm, atrial sensing occurs and the ventricles are paced after an appropriate AV interval. When episodes of AF occur, the pacemaker mode switches and paces the ventricle at a steady rate.
4.
DC cardioversion of AF can be a reasonable treatment for the first episode or for patients with infrequent episodes. DC cardioversion is safe in the absence of digoxin toxicity or hypokalaemia, but is associated with a risk of embolism if the patient’s AF has been present for more than 48 hours. In this case, 1 month’s therapeutic anticoagulation should be instituted before the procedure and continued for 4 weeks afterwards. An alternative is to perform a transoesophageal echocardiogram to look for left atrial
appendage thrombus or spontaneous echocardiograph contrast (a sign of slow blood flow). The absence of these means that DC cardioversion is safe, but that warfarin must be given for 4 weeks afterwards because there is a persisting risk over this period.
5.
Reversion of AF with drug treatment is difficult. Many episodes terminate spontaneously but drug treatment is given the credit. It is known that digoxin does not increase the reversion rate, but the class III drugs and flecainide do improve the chances somewhat. Sometimes control of the heart rate and awaiting spontaneous reversion can be an option. A decision to go on to DC cardioversion, however, should be made before 48 hours has passed.
6.
Over many years attempts have been made to prevent AF by surgical or catheter ablation techniques. Pulmonary vein isolation is now commonly performed for intractable symptomatic AF. Radiofrequency energy is used to isolate the two pairs of pulmonary veins in the left atrium. The rationale for this approach is that almost all AF seems to be initiated by electrical activity arising from this part of the heart. Isolation of this area from the rest of the heart prevents the initiation of AF. The procedure is complicated and time-consuming (4–6 hours per case). It is not a practical solution for most cases of AF. Success rates of about 60% are usually quoted. Until recently, an uncommon but severe complication involved the late occurrence of pulmonary vein stenosis. Newer techniques have made this a rare problem. Other complications include heart block and cardiac perforation. Successful treatment possibly spares a patient the need for anticoagulation.
7.
Protecting patients from embolic events is perhaps the most important aspect of the management of AF. Cerebral embolus is the most feared complication, but life-threatening peripheral embolisation (e.g. to the mesenteric bed) can occur. Patients should have this aspect of AF explained to them early on. The risk of embolism is low in people under the age of 60 and without any risk factors: <0.5% a year. It can be as high as 30% for patients with mitral stenosis. The most recent advice has been to anti-coagulate unless a patient seems at really low risk.
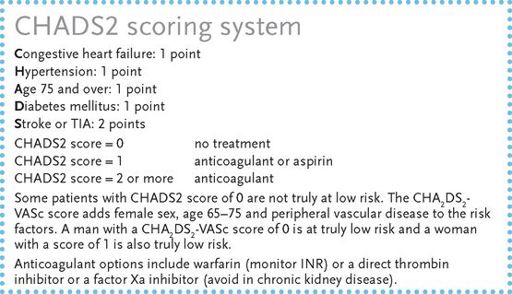
Use the
CHADS2
or CHA
2
DS
2
-VASc scoring system to help you decide whom to anticoagulate with AF:
Remember that episodes of AF, for example, on a Holter monitor or at pacemaker interrogation, must last longer than 30 seconds to be considered significant.
8.
Patients with risk factors remain at risk of stroke even if sinus rhythm has been restored. Those with self-limiting paroxysmal AF are also at risk if episodes are more than a rare event. Aspirin gives some protection to those unwilling or unable to take warfarin. The combination anti-platelet treatment (e.g. with aspirin and clopidogrel) is somewhat more effective than aspirin alone, but is inferior to warfarin (and dual anti-platelet drugs increase the risk of gut bleeds).
9.
An assessment of the patient’s ability to manage regular blood tests and dosage adjustments is necessary before treatment can begin. Patients are often reluctant to undertake the complexities of treatment but should not be allowed to decline treatment until all the risks of this approach have been carefully explained.
10.
The availability of home international normalised ratio (INR) testing machines that use a capillary blood sample has made the use of warfarin more acceptable to some patients (e.g. those who travel frequently). A number of studies have shown that this approach is safe for selected patients. The safe therapeutic range is an INR of between 2 and 2.5.
11.
Find out from the patient how the warfarin is managed and whether he or she knows the last few readings and dosage. Patients should be encouraged to keep a record of their INR results and warfarin doses. The examiners will expect considerable detail about the patient’s warfarin management.
12.
Novel oral anti-thrombotic agents are available. The first of these, dabigatran, is an oral anti-thrombin drug with similar efficacy to warfarin. The drug is effective within a few hours of the first dose but has to be taken twice a day. The larger dose (150 mg) is recommended for people under the age of 70 unless they have chronic kidney disease. Bleeding (especially gastrointestinal bleeding) has been a problem for patients especially on the larger dose over age 70 or if they have chronic kidney disease. It is associated with a higher risk of myocardial infarction. Gastrointestinal side-effects are common. The drug does not need monitoring. It is not indicated for valvular AF or for patients with mechanical valve replacements.
There are also the anti-factor Xa agents, e.g. rivaroxiban and apixaban. Rivaroxiban is taken once a day. The usual dose is 20 mg. Some authorities recommend 15 mg for patients with moderate renal impairment. Apixaban is taken as a 5 mg dose twice a day or 2.5 mg twice a day for patients over 80 or with moderate renal impairment. None of these drugs is indicated for patients with severe kidney failure. None is easily reversed, although dabigatran can be dialysed.
CHAPTER 6
The respiratory long case
I here present the reader with a new sign, which I have discovered for detecting diseases of the chest. This consists in percussion …
Leopold Auenbrugger (1760)
Bronchiectasis
Bronchiectasis is a reasonably common subject for a long case and usually poses a management problem. It is defined as pathological and permanent dilatation of the bronchi. There are associated destructive and inflammatory changes in the walls of the segmental and subsegmental bronchi. The diagnosis is not always straightforward because there are overlap syndromes, e.g. COPD, asthma and chronic bronchitis (
Table 6.1
).
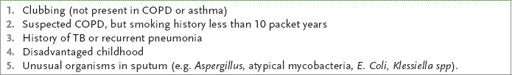
Table 6.1
Features suggesting predominate bronchiectasis
The history
1.
Find out when the patient’s respiratory problems began. Classically the cough and sputum begin in childhood, although adult onset is becoming more common. Ask about childhood whooping cough or measles. Lower respiratory tract infection with influenza and adenoviruses is an increasingly common cause of the disease. Potentially necrotising bacteria are also a cause if antibiotic treatment is inadequate – these include
Staphylococcus aureus
and
Klebsiella
organisms. The abnormal pulmonary defence mechanisms, or mucus clearance, associated with cystic fibrosis, tuberculosis, immunoglobulin deficiency, HIV infection and primary ciliary dyskinesia (immotile cilia syndrome) make these important causes of the condition. Localised bronchiectasis can occur in association with a space-occupying lesion, which can be endobronchial or external.
Symptoms include:
a.
recurrent haemoptysis
b.
dyspnoea and wheeze
c.
chronic sinusitis (70%)
d.
recurrent pneumonia and pleurisy
e.
systemic symptoms of weight loss, fever and anorexia
f.
symptoms of right heart failure – a late event.
2.
Ask about recent precipitating causes of admissions to hospital (e.g. infection, haemoptysis).
3.
Enquire about treatment – physiotherapy, postural drainage, antibiotics (as prophylaxis or treatment), bronchodilators, lung resection.
4.
Determine whether the patient had childhood immunisations (e.g. MMR).
5.
Ask about investigations in the past (e.g. CT scanning, ciliary function studies, sweat test, bronchograms (memorable!)).
6.
Establish aetiology, such as childhood or early adult infections (e.g. pneumonia, measles, whooping cough) (
Table 6.2
). The majority of cases have no obvious cause if those due to cystic fibrosis are excluded.