How to Read a Paper: The Basics of Evidence-Based Medicine (31 page)
Read How to Read a Paper: The Basics of Evidence-Based Medicine Online
Authors: Trisha Greenhalgh
This is an extreme example, but within the past few years I have seen guidelines for treating constipation in the elderly that offered no alternative to the combined insults of large amounts of bran and twice-daily suppositories. Small wonder that the district nurses who were issued with them (for whom I have a good deal of respect) have gone back to giving castor oil.
For a further discussion on how to incorporate the needs and priorities of patients in guideline development, see a recent review [20].
Question Ten: Does the guideline include recommendations for its own dissemination, implementation and regular review?
Given the well-documented gap between what is known to be good practice and what actually happens (see preceding text), and the barriers to the successful implementation of guidelines discussed in section ‘How can we help ensure that evidence-based guidelines are followed?’, it would be in the interests of those who develop guidelines to suggest methods of maximising their use. If this objective were included as standard in the ‘Guidelines for good guidelines’, the guideline writers' output would probably include fewer ivory tower recommendations and more that are plausible, possible and capable of being explained to patients. Having said that, one very positive development in EBM since I wrote the first edition of this book is the change in guideline developers' attitudes: they now often take responsibility for linking their outputs to clinicians (and patients) in the real world and for reviewing and updating their recommendations periodically.
References
1
Swinglehurst D. Evidence-based guidelines: the theory and the practice.
Evidence-Based Healthcare and Public Health
2005;
9
(4):308–14.
2
Shekelle P, Woolf S, Grimshaw JM, et al. Developing clinical practice guidelines: reviewing, reporting, and publishing guidelines; updating guidelines; and the emerging issues of enhancing guideline implementability and accounting for comorbid conditions in guideline development.
Implementation Science
2012;
7
(1):62.
3
Gurses AP, Marsteller JA, Ozok AA, et al. Using an interdisciplinary approach to identify factors that affect clinicians' compliance with evidence-based guidelines.
Critical Care Medicine
2010;
38
:S282–91.
4
Gagliardi AR, Brouwers MC, Palda VA, et al. How can we improve guideline use? A conceptual framework of implementability.
Implementation Science
2011;
6
(1):26.
5
Evans-Lacko S, Jarrett M, McCrone P, et al. Facilitators and barriers to implementing clinical care pathways.
BMC Health Services Research
2010;
10
(1):182.
6
Michie S, Johnston M. Changing clinical behaviour by making guidelines specific.
BMJ: British Medical Journal
2004;
328
(7435):343.
7
Grol R, Dalhuijsen J, Thomas S, et al. Attributes of clinical guidelines that influence use of guidelines in general practice: observational study.
BMJ: British Medical Journal
1998;
317
(7162):858–61.
8
Evans JG. Evidence-based and evidence-biased medicine.
Age and Ageing
1995;
24
(6):461–3.
9
Allen D, Harkins K. Too much guidance?
The Lancet
2005;
365
(9473):1768.
10
Merenstein D. Winners and losers.
JAMA: The Journal of the American Medical Association
2004;
291
(1):15–6.
11
Grimshaw JM, Russell IT. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations.
The Lancet
1993;
342
(8883):1317–22.
12
Harrison MB, Légaré F, Graham ID, et al. Adapting clinical practice guidelines to local context and assessing barriers to their use.
Canadian Medical Association Journal
2010;
182
(2):E78–84.
13
Grimshaw J, Thomas R, MacLennan G, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies.
International Journal of Technology Assessment in Health Care
2005;
21
(01):149.
14
Eccles M, Grimshaw J, Walker A, et al. Changing the behavior of healthcare professionals: the use of theory in promoting the uptake of research findings.
Journal of Clinical Epidemiology
2005;
58
(2):107–12.
15
Eccles MP, Grimshaw JM, MacLennan G, et al. Explaining clinical behaviors using multiple theoretical models.
Implementation Science
2012;
7
:99.
16
Davies P, Walker AE, Grimshaw JM. A systematic review of the use of theory in the design of guideline dissemination and implementation strategies and interpretation of the results of rigorous evaluations.
Implementation Science
2010;
5
:14.
17
Brouwers MC, Kho ME, Browman GP, et al. AGREE II: advancing guideline development, reporting and evaluation in health care.
Canadian Medical Association Journal
2010;
182
(18):E839–42.
18
Thomson R, Lavender M, Madhok R. How to ensure that guidelines are effective.
BMJ: British Medical Journal
1995;
311
(6999):237–42.
19
Gabbay J, May Al. Evidence based guidelines or collectively constructed “mindlines?” Ethnographic study of knowledge management in primary care.
BMJ: British Medical Journal
2004;
329
(7473):1013.
20
Boivin A, Currie K, Fervers B, et al. Patient and public involvement in clinical guidelines: international experiences and future perspectives.
Quality and Safety in Health Care
2010;
19
(5):1–4.
21
Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables.
Journal of Clinical Epidemiology
2011;
64
(4):383–94.
22
Hill J, Bullock I, Alderson P. A summary of the methods that the National Clinical Guideline Centre uses to produce clinical guidelines for the National Institute for Health and Clinical Excellence.
Annals of Internal Medicine
2011;
154
(11):752–7.
23
Aarts MC, van der Heijden GJ, Rovers MM, et al. Remarkable differences between three evidence-based guidelines on management of obstructive sleep apnea-hypopnea syndrome.
The Laryngoscope
2013;
123
(1):283–91.
Chapter 11
Papers that tell you what things cost (economic analyses)
What is economic analysis?
An economic analysis can be defined as
one that involves the use of analytical techniques to define choices in resource allocation
. Most of what I have to say on this subject comes from advice prepared by Professor Michael Drummond's team [1] for authors and reviewers of economic analyses as well as the excellent pocket-sized summary by Jefferson et al. [2], both of which emphasise the importance of setting the economic questions about a paper in the context of the overall quality and relevance of the study (see section ‘Ten questions to ask about an economic analysis’).
The first economic evaluation I ever remember was a TV advertisement in which the pop singer Cliff Richard tried to persuade a housewife that the most expensive brand of washing-up liquid on the market ‘actually works out cheaper’. It was, apparently, stronger on stains, softer on the hands and produced more bubbles per penny than ‘a typical cheap liquid’. Although I was only nine at the time, I was unconvinced. Which ‘typical cheap liquid’ was the product being compared with? How much stronger on stains was it? Why should the effectiveness of a washing-up liquid be measured in terms of bubbles produced rather than plates cleaned?
Forgive me for sticking with this trivial example, but I'd like to use it to illustrate the four main types of economic evaluation that you will find in the literature (see
Table 11.1
for the conventional definitions).
- Cost-minimisation analysis
: ‘“Sudso” costs 47 p per bottle whereas “Jiffo” costs 63 p per bottle’. - Cost-effectiveness analysis
: ‘“Sudso” gives you 15 extra clean plates per wash than “Jiffo”’. - Cost–utility analysis
: ‘In terms of quality-adjusted homemaker hours (a composite score reflecting time and effort needed to scrub plates clean, and hand roughness caused by the liquid), “Sudso” provides 29 units per pound spent, whereas “Jiffo” provides 23 units’. - Cost–benefit analysis
: ‘The net overall cost (reflecting direct cost of the product, indirect cost of time spent washing up, and estimated financial value of a clean plate relative to a slightly grubby one) of “Sudso” per day is 7.17p, while that of “Jiffo” is 9.32p’.
Table 11.1
Types of economic analysis
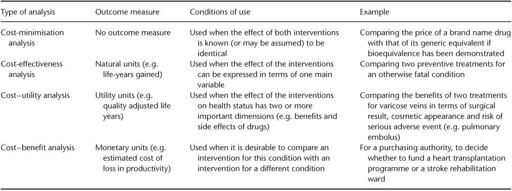
You should be able to see immediately that the most sensible analysis to use in this example is cost-effectiveness analysis. Cost-minimisation analysis (see
Table 11.1
) is inappropriate as ‘Sudso’ and ‘Jiffo’ do not have identical effectiveness. Cost–utility analysis is unnecessary because, in this example, we are interested in very little else apart from the number of plates cleaned per unit of washing-up liquid—in other words, our outcome has only one important dimension. Cost–benefit analysis is, in this example, an absurdly complicated way of telling you that ‘Sudso’ cleans more plates per penny.
There are, however, many situations where health professionals, particularly those who purchase health care from real cash-limited budgets, must choose between interventions for a host of different conditions whose outcomes (such as cases of measles prevented, increased mobility after a hip replacement, reduced risk of death from heart attack or likelihood of giving birth to a live baby) cannot be directly compared with one another. Controversy surrounds not just how these comparisons should be made (see section ‘How can we help ensure that evidence-based guidelines are followed?’), but also who should make them, and to whom the decision-makers for the ‘rationing’ of health care should be accountable. These essential, fascinating and frustrating questions are beyond the scope of this book, but if you are interested I recommend a recent book by Donaldson and Mitton [3].
Measuring costs and benefits of health interventions
A few years ago, I was taken to hospital to have my appendix removed. From the hospital's point of view, the cost of my care included my board and lodging for 5 days, a proportion of doctors' and nurses' time, drugs and dressings and investigations (blood tests and a scan). Other
direct costs
(see Box 11.1) included my general practitioner's time for attending to me in the middle of the night and the cost of the petrol my husband used when visiting me (not to mention the grapes and flowers).
In addition to this, there were the
indirect
costs of my loss in productivity. I was off work for 3 weeks, and my domestic duties were temporarily divided between various friends, neighbours and a nice young girl from a nanny agency. And, from my point of view, there were several
intangible
costs, such as discomfort, loss of independence, the allergic rash I developed on the medication and the cosmetically unsightly scar that I now carry on my abdomen.
As Box 11.1 shows, these direct, indirect and intangible costs constitute one side of the cost–benefit equation. On the benefit side, the operation greatly increased my chances of staying alive. In addition, I had a nice rest from work, and, to be honest, I rather enjoyed all the attention and sympathy. (Note that the ‘social stigma’ of appendicitis can be a positive one. I would be less likely to brag about my experience if my hospital admission had been precipitated by, say, an epileptic fit or a nervous breakdown, which have negative social stigmata).