i bc27f85be50b71b1 (260 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown
APPt..NDIX 111-8: MECHANICAL VENllLATION 827
which the panent attempts each wean (time of day, activities before and
after the wean, position during the wean) and parameters to be manipulated during the wean (frequency, intensity, duration). Patients should be placed in a position that facilitates the biomechanics of their ventilation.12 For many parients, rhis is seared and may also include the ability ro sir forward with the arms supported.
Biofeedback to increase VT and relaxation has been shown to
improve rhe effecriveness of weaning and reduce time on the ventilaror. n Inspirarory muscle resistive training has also been shown to increase respiratory muscle strength and endurance ro facilitate the
weaning success. 14
References
I. Manno P. The ICU Book (2nd ed). Philadelphia: Lea & Febiger, 1998.
2. Slutsky AS. Mechanical ventilation. American College of Chest Physicians' Consensus Conference Isee commentsJ. Chest 1993; 104: 1833.
3. Howman SF. Mechanical vemilation: a review and update for clinicians.
Hosplt.1 Physician 1999;December:26-36.
4. Sadowsky liS. Thoracic Surgical Procedures, Monitoring, and Support
Equipment. In EA Hillegass, HS Sadowsky (eds), Essentials of Cardiopulmonary PhYSIcal Therapy (2nd ed). Philadelphia: Saunders, 2001; 464-469.
5. Amuero A, Peters JI, Tob," MJ, et al. Effecrs of prolonged mechanical
ventilation on diaphragmatic function in healthy adult baboons. Crit
Care Med 1997;25:1187-1190.
6. Gerold KB. Physical therapists' guide to the principles of mechanical
ventilation. Cardlopul Phys Ther 1992;3:8.
7. Costello ML, Mathieu-Costello 0. West JB. Stress fracture of alveolar
epithelial cells studied by scanning electron microscopy. Am Rev Respir
DIS 1992;145:1446-1455.
8. Mathieu-Costello 0, West JB. Are pulmonary capillaries susceptible to
mechal1lcal stress? Chest 1994;105(Suppl):1025-107S.
9. Heimler R, Huffman RG, Starshak RJ. Chronic lung disease in premature infams: A retrospective evaluation of underlying factors. Crit Care Med 1988;16:1213-1217.
10. Yang KL, Tobin MJ. A prospective study of indexes predicting the outcome of trials of weaning from mechanical vencilation. N Engl J Med 1991 ;324: 1446-1495.
11. Dries DJ. \Veaning from mechanical ventilation. J Trauma 1997;
43:372-384.
12. Shekleron ME. Respiratory muscle condition and the work of breachinga critical balance in [he weaning patient. AACN Clin Issues Crit Care 1991;2:405-414.

828 AC� CARE HANDBOOK FOR PHYSICAL THERAPISTS
13. Holliday JE, Hyers TM. The reduction of wean time frol11 mechanical
ventilation using tidal volume and relaxation biofeedback. Am Rev
Respir Dis 1990;141:1214-1220.
14. Aldrich TK, Karpel JP, Uhrlass RM, et 301. Weaning from mechanical
ventilation: adjunctive use of inspiratory muscle resistive training. Crit
Care Med 1989;17:143-147.


III-C
Circulatory Assist Devices
Jaime C. Paz
The purpose of this appendix is to describe rhe following circulatory
assist devices: (1) intra-aortic balloon pump (IABP), (2) vemricular
assist device (VAD) , and (3 ) extracorporal membrane oxygenarion
(ECMO) . These devices are primarily used wirh a patient who has
severe cardiac pump dysfunction, with or without concurrent pulmonary pump dysfuncrion.
Intra-Aortic Balloon Pump
The main function of rhe IABP is to lessen rhe work (decreased myocardial oxygen demand) of rhe heart by decreasing afrerioad in the proximal aorta. The LABP also improves coronary artery perfusion
(increa ed myocardial oxygen supply) by increasing diasrolic pressure
in the aorta,l,2
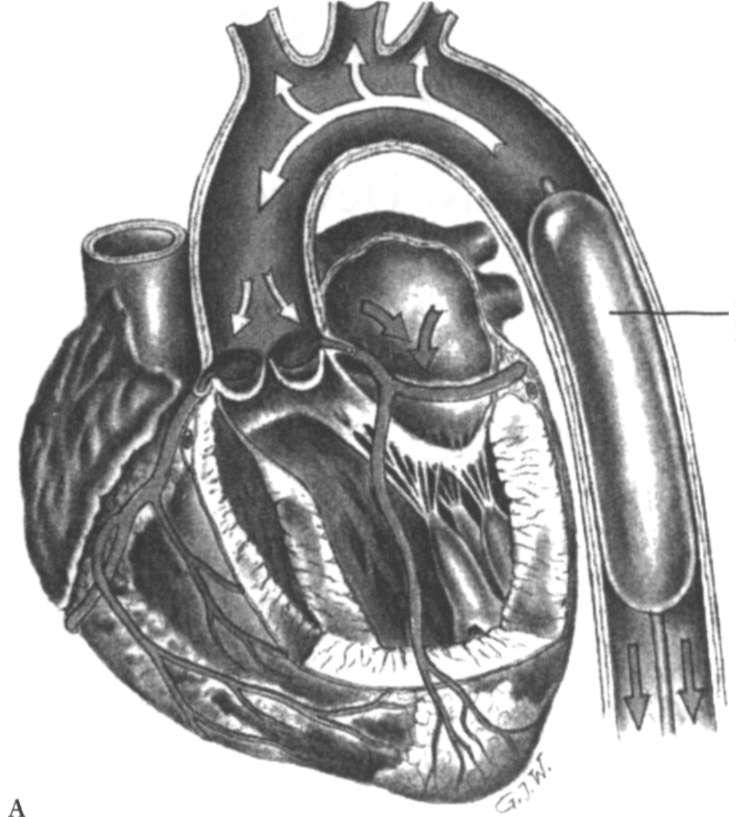
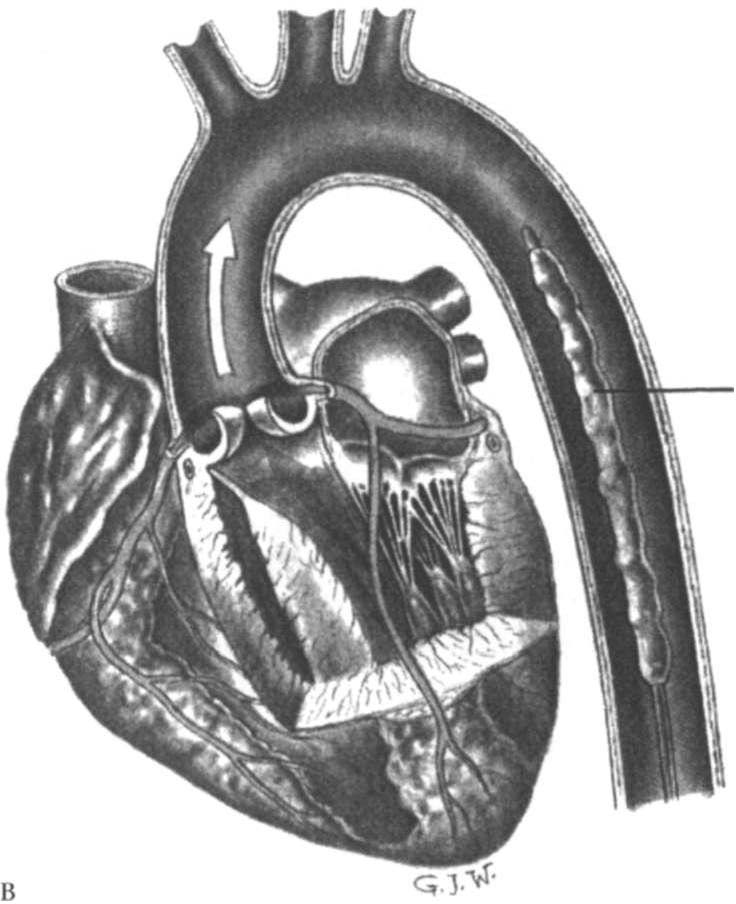
The IABP consists of a carheter with a sausage-shaped balloon ar
the end of ir, all of which is connecred to an external pump-controlling device. The catheter is inserted percutaneously or surgically into the femoral artery and is threaded amegrade umil ir reaches the proximal descending thoracic aorta. Figure III-C.! illustrates the balloon 829

830 ACUTE CARE HANDBOOK FOR PHYSICAL TIIFRAPISTS
Balloon
inflated
Figure HI-C. I. Mechanisms of action of imra-aortic balloon pump. A. Diastolic balloon inflation augments coronary blood flolll. B. Systolic balloon deflation decreases afterload. (Reprinted tvith permission from LA Thelan
{edl. Critical Care Nursing: Diagnosis and Management (2nd edJ. St. Louis:
Mosby, 1994.)
inflating during ventricular filling (diastole) and deflating during ventricular contraction (systole). The deflation of the balloon juSt before aortic valve opening decreases afterload and therefore reduces resistance to the ejection of blood during systole. The blood in the aorta is then propelled forward into the systemic circulation. The inflation of
the balloon during diastole assists with the perfusion of the coronary
and cerebral vessels. This process is referred to as counterpulsation,
because the inflation and deflation of the balloon occur opposite to
the contraction and relaxation of the heart. 1.2

API'F.NDIX III�C: CIRCULATORY ASSIST DEVICES
831
Balloon
deflated
Indications for IABI' include the following:
•
Acute left ventricular failure
•
Unstable angina
•
Status post acute myocardial infarction
•
Cardiogenic shock
•
Papillary muscle dysfunction with resultant mitral valve regurgitation
•
Ventricular septal defect