i bc27f85be50b71b1 (261 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown

832 AClITE CARE HANDBOOK FOR I'HYSICAL THERAPISTS
•
Refractory ventricular dysrhyrhmias
•
Anticipated heart transplantation
The ratio of heart beats to counterpulsations of the [ABP indicates the
amount of circulatory suppOrt an individual requires (e.g., 1 to I is
one counterpulsation to one heart beat; 1 to 4 is one counterpulsation
to every fourth heart beat; a ratio of 1 to 1 provides maximum circulatory suPPOrt). Weaning from IABP involves gradually decreasing the number of counterpulsarions to heart beats, with the goal being one
counterpulsation for every fourth heart beat, as tolerated, before discontinuing the IABP. Although weaning from the lABP is generally performed by decreasing the number of counterpulsations, weaning
can also be performed by gradually decreasing the amount of inflation
pressure of the balloon in the aorta.',2
The following are complications of IABP:
•
Ischemia of the involved limb secondary to occlusion of femoral
artery from compression or from thrombus formation
•
Slippage of the balloon, resulting in occlusion of subclavian or
renal arteries
Clinical Tip
•
During IABP, the lower extremity in which femoral
access is obtained cannot be flexed at the hip, and the
patienr's head cannot be raised higher than 40 degrees in
bed.
•
Depending on the amount of time spent on the pump,
the patient may require active-assistive range of motion
exercises for hip flexion after the IABP is removed.
Ventricular Assist Device
A VAD is a mechanical pump that provides prolonged circulatory
assistance in patients who have ventricular failure from myocardial
infarction or are awaiting transplantation because of severe cardiomyopathy. The mechanical pump can be internal or external to the


APPENDIX III-C: CIRCULATORY ASSIST DEVICES
833
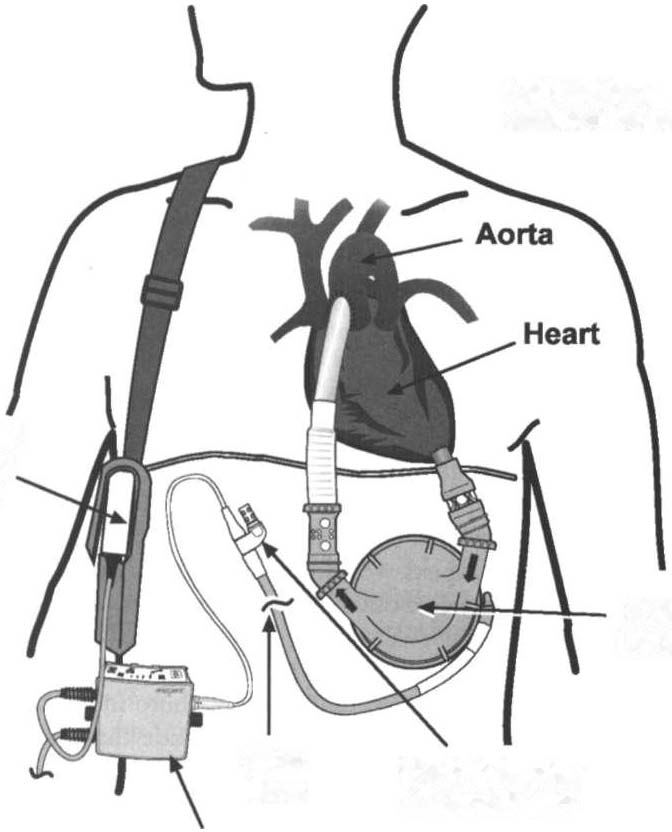
patient. An internal VAD consists of a pump that is surgically placed
extra peritoneally within the patient's abdominal cavity with access
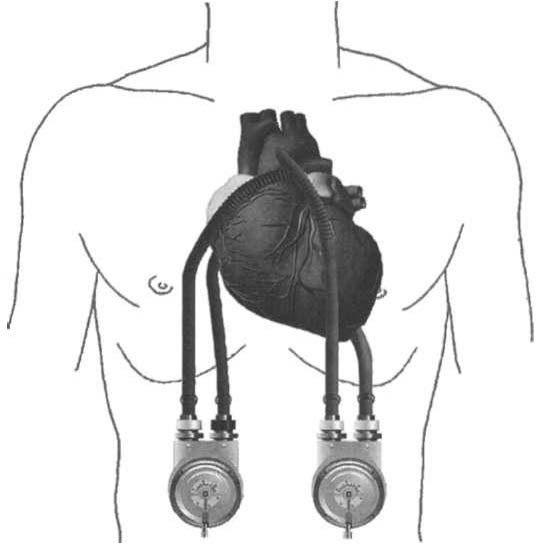
lines leading to an ex ternal control device. An external VAD consists
of a pump that is completely ex ternal to the patient, bur with access
lines shunting blood from the heart to the great vessels.2"
Figures III-C.2 and III-C.3 illustrate an example of an internal
VAD and an ex ternal VAD, respectively. Generally, the left ventricle is
most commonly assisted (left VAD [LVADO, but occasionally, the
Left Battery
omitted for clarity
External
Battery
Pack
/
XVE
LVAD
Skin
Vent Adapter
Line
& Vent Filter
XVE System
Controller
Figure IU-C.2. The HeartMate implantable left ventricular assist device
(LVAD). (XVE extended lead vented electric.) (Reprinted with permission
=
{rom Thoratec Corporation, Woburn, MA.}

834 ACUTE CARE HANDBOOK FOR PHYSICAL THERAPISTS
Figure m-C.3. The Thoratec paracorporeal ventricular assist device.
(Reprinted with permission from Thoratec Corporation, Wobunt, MA.)
right ventricle also needs assistance (right VAD). In more severe situations, both ventricles need to be assisted (bivenrricular assist device) .
The various types and general characteristics of internal and external
VADs are described briefly in Table Ill·c.l. It is beyond the scope of
this appendix to describe in detail all the aspects of each type of VAD;
however, physical therapists working with patients on a VAD need to
be familiar wirh the type of machine that the patient is on, as well as
the safery features of the VAD.
Weaning from VAD involves a gradual decrease in flow rates,
which allows the patient's ventricle to contribute more to rotal systemic circulation. Complications of VAD include thrombosis, bleeding, and infection at or near the insertion sites of the access lines.
The combination of technological advancements and a lack of donor
organs has increased the use of VADs in patientS with cardiomyopathy.
Therefore, physical therapists are more likely to encounter rhis equip·
ment in the hospital. Research has demonstrated that patients with a
VAD can be mobilized safely in the hospital and that their exercise tolerance can be improved while awaiting transplantation.�



