i bc27f85be50b71b1 (281 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown
In patients with upper-extremity amputation, a sling may
be used to help manage edema.
Phantom limb
Often described as a cramping, squeezing, shoming, or
pain
burning pain felt in the part of the extremity that has
been removed. The physical therapist may use
desensitizing techniques (e.g., massaging the residual
limb), exercise, hot and cold therapy, electrical
stimulation, or other modalities when phantom limb
pain is determined as the cause of the patient's pain.
Hypersensitivity
Patient should be encouraged to rub the residual limb with
increasing pressure as tolera[ed.
Skin condition
Ensure stability of new incision(s) before, during, and
after physical therapy intervention. Examine the incision for any changes in [he appearance (size, shape,
open areas, color), temperature, and moisture level.
Instruct patient and nursing staff on importance of frequent position changes to prevent skin breakdown.
Implement out-of-bed activities as soon as possible.
Instruct patient in active movements and bed mobility
activities such as bridging, rolling, and moving up and
down in the bed.
Sources: 03ra from B Engslrom, C Van de Ven (eds). Thcrapy for Ampurees (3rd cd).
Edinburgh, UK: Churchill Livingsrone, 1999j27-37, 43-45; B May (cd). Amputations
and Prosrhcrics: A Case Study Approach. Phibdelphia: FA Davis, 1996;73,86-88; and
SN Banerjee (cd). Rehabilirarion Management of Ampurees. Balrimore: Williams &
W;lk;ns, 1982;30-33, 255-258.


APPENDIX VII: AMPlffATION
895
Table VII-4. Specific Considerations and Treatment Suggestions for
Patients with Upper- or Lower-Extremiry Amputation
Consideration
Treatment Suggestions
Joint
Upper extremiry
conrracture
Physical therapy should consist of active movements of all
of the joints above the level of the amputation,
including movementS of the scapula. Patients who use
upper-extremity slings to fixate the arm in elbow
flexion and shoulder internal rotation should be
examined regularly for contractu res.
Lower extremity
The physical therapist should provide the patient and
members of the nursing scaff with education on residual
limb positioning, proper pillow placement, and the use
of splint boards.
Patients with a below-the-knee amputation will be mOst
susceptible to knee flexion contraction. A pillow should
be placed under the tibia rather than under the knee to
promote extension.
Patients with above-the-knee amputations or disarticulations will be most susceptible to hip flexor and
abductor contractures.
The physical therapist should begin active range-of-motion
exercises and provide passive stretching as indicated.
Decreased
Upper extremiry
functional
During ambulation, patients tend to flex their tfunk
mobility
roward the side of the amputation and maintain a stiff
gait panern that lacks normal arm swing. Patients often
need gait, balance, posture retraining, or a combination
of these.
It is important to work on active movements, specifically
the movements that might be used for powering a prosthesis, such as in [he following:
Transradial body powered prosthesis: elbow extension,
shoulder flexion, shoulder girdJe protraction. or a
combination of these
Transhumeral body powered prosthesis: elbow flexion,
shoulder extension, internal rotation, abduction and
shoulder girdle protraction and depression.

896 AClITE CARE HANDBOOK FOR PHYSICAL THERAPISTS
Table VU 4. Continued
-
Consideration
Treannenr Suggestions
Lower extremity
Techniques should range from bed mobiliry training to
transfer training to ambulation or wheelchair mobility.
Patients with bilateral above-knee amputacions will
need a custom wheelchair that places the rear axle in a
more posterior position to compensate for the
alteration in the patient's center of gravity when sitting.
Sources: Data from LA Karacoloff, FJ Schneider (cds). Lower Extrcmity Ampmation: A
guide to Functional Outcomes in Physical Therapy Managcmcnt. Rockville, MD:
Aspen, 1985; B Engstrom, C Van de Ven (cds). Therapy for Amputees (3rd cd). Edinburgh, UK: Churchill Livingstone, J999;27-37, 43-45, 243-257; B May (ed). Amputations and Prosthetics: A Case Srudy Approach. Philadelphia: FA Davis, 1996;86-88; SN Banerjee (cd). Rehabiliration Managemcll( of Amputees. Baltimore: Williams &
Wilkins, 1982;30-33,255-258; and R Ham, L Cofton (cds). Limb Ampuration: From
Aetiology to Rehabilitation. London: Chapman & Hall, 1991;136-143.
References
I. Engsrrom B, Van de Ven C (cds). Therapy for Ampurees (3rd cd). Edinburgh, UK: Churchill Livingsrone, 1999;27-37, 43-45, 149-150, 187-188, 208.
2. Karacoloff LA, Schneider FJ (eds). Lower Exrremiry Amputation: A
Guide to Functional Outcomes in Physical Therapy Management. Rockville, MD: Aspen, 1985.
3. Thompson A, Skinner A, Piercy J (eds). Tidy's Physiotherapy (12th ed).
Oxford, UK: Butterworth-Heinemann, 1992;260.

VIII
Postural Drainage
Michele P. West
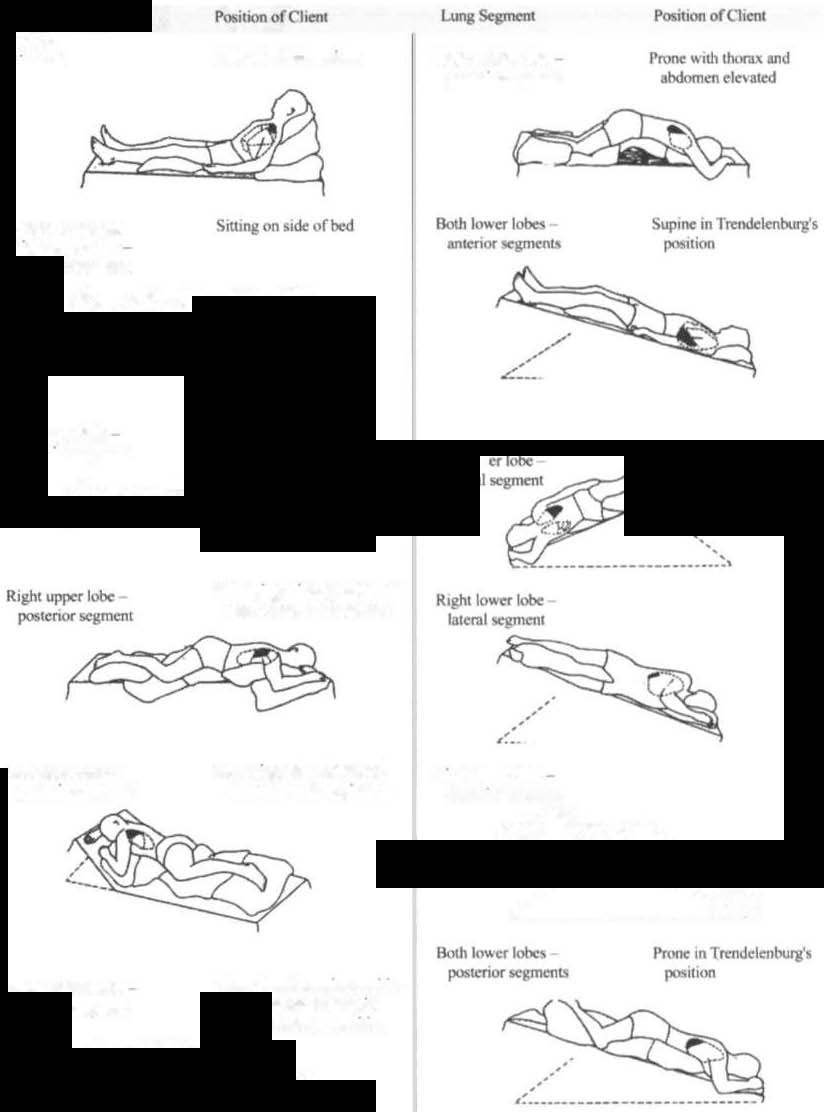
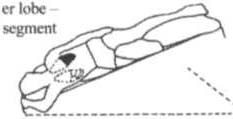
Postural drainage is the positioning of a patient with an involved lung
segment as close to perpendicular to the Aoot as possible to facilitate
the drainage of bronchopulmonary secretions.' Figure Vlll-] demonstrares the various postural drainage positions most applicable in the acute care setting. The lise of postural drainage as an adjunct to other
techniques (mainly breathing and coughing exercises, vibration, shaking, and percussion) can be highly effective for mobilizing retained secretions and maximizing gas exchange. The physical therapist
should note that there are many clinical contraindicarions and considerations for postural drainage that may require position modification to maximize patient safety, comfort, and tolerance.
The contraindications for the use of Trendelenburg (placing the
head of the bed in a downward position) include the following2•3:
•
Patients in which an increase in intracranial pressure should be
avoided
•
Uncontrolled hypertension
• Uncontrolled or unprotected airway with a risk of aspiration
•
Recent gross hemoptysis
897