i bc27f85be50b71b1 (90 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown
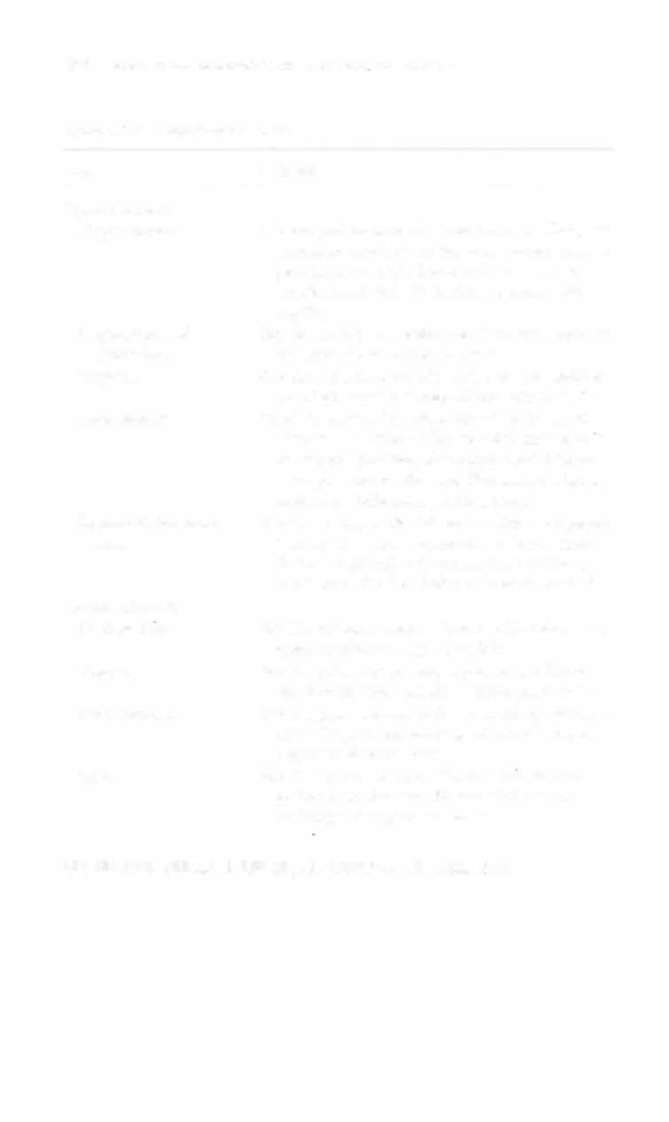
Table 4-16 outlines rhe method of sensarion resting by stimulus.
Table 4-16. Sensation Testing
Sensation
Modality and Method
Superficial pain
Touch a pin or pen cap over the cxuemities or trunk.
Deep pain
Squeeze rhe parienr's forearm or calf bulk.
Light touch
Apply Iighr pressure with rhe finger, a cotton ball, or
washcloth over rhe extremities or trunk.
Proprioceprion
Lightly grasp the distal inrerphalangeal joinr of the
patienr's finger or great tOC, and move the joint slowly
up and down. Ask the patient to state in which direction the joinr is moved. Test distal to proximal
(e.g., roe ro ankle to knee).
Vibrarion
Activate a tuning fork and place on a bony prominence.
Ask the patient to state when the vibration slows and
stops. Proceed distal co proximal.
Temperacure
Place test tubes filled with warm or cold water on [he
area of the patient's body to be tested. Ask the patient
to state the temperature. ( Rarely done in the acute care
serring.)
Stereognosis
Place a familiar object in the patient'S hand and ask the
patient to identify it.
Two-poinr
Place two-point caliper or drafting compass on area ro be
discriminarion
tested. Ask the patient to distinguish whether it has
one or two points.
Graphesrhesia
Trace a lerrer or number in the patient's open palm and
ask the patient co state what was drawn.
Double
Simultaneously couch tViO areas on the same side of the
simultaneous
patient's body. Ask patient to locate and distinguish
stimulation
both points.
Sources: Data from KW Lindsay, I Bone, R Callander (cds). Neurology and Neurosurgery
lIIustr:ned (2nd cd). Edinburgh, UK: Churchill Livingstone, 1991; S Gilman, SW Newman (cds). Manter and Gatt's Essentials of Clinical Neuroanatomy and Neurophysiology (7th ed). Philadelphia: FA Davis, 1 989; and JV Hickey (cd). The Clinical Practice of Neurological and Neurosurgical Nursing (4th ed). I)hiladelphia: Lippincon, 1 997.




NERVOUS SYSTEM
299
Clinical Tip
Before completing the sensory examination, the physical
therapist should be sure that the patient can correctly identify stimuli (e.g., that a pinprick feels like a pinprick).
Coordination
Although each lobe of the cerebellum has its own function, cootdination tests cannot truly differentiate among them. Coordination tests evaluate the presence of ataxia (general incoordination), dysmetria
(overshooting), and dysdiadochokinesia (inability to perform rapid
alternating movements) with arm, leg, and trunk movements, as well
as with gait.8 The results of each test (Table 4- 1 7) are described in
tetms of the patient's ability to complete the test, accuracy, tegularity
of rhythm, and presence of tremor."
Another test is the prol1ator drift test, which is used to qualify loss
of position sense. While the patient is sitting or standing, he or she
flexes both shoulders and extends the elbows with the palms upward.
The patient is then asked to close his or her eyes. The forearm is
observed for 1 0-20 seconds for ( 1 ) pronation or downward drift,
which suggests a contralateral corticospinal lesion, or (2) an upward
or sideward drift, which suggests loss of position sense H
Diagnostic Procedures
A multitude of diagnostic tests and procedures is used to evaluate, differentiate, and monitOr neurologic dysfunction. Each has its own cost, accuracy, advantages, and disadvantages. For the purposes of
this text, only the procedures most commonly used in the acute care
setting are described.
X-Ray
X-rays can provide anterior and lateral views of the skull that are
used to assess the presence of calcification, bone erosion, or fracture,
especially after head or facial trauma or if a tumor is suspected. Anterior, lateral, and posterior views of the cervical, thoracic, lumbar, and sacral spine are used to assess the presence of bone erosion, fracture,