Knocking on Heaven's Door: The Path to a Better Way of Death (24 page)
Read Knocking on Heaven's Door: The Path to a Better Way of Death Online
Authors: Katy Butler
Tags: #Non-Fiction
ing conditions that the Victorian-era nursing reformer Florence
Nightingale considered essential: quiet, rest, and fresh air. Of
those who suffer hospital delirium, 35 percent to 40 percent die
within a year.
My mother called me, weeping. She was exhausted. The
hospital was neglecting him. She was afraid to drive alone to
New Haven. She didn’t know what to do. She needed a driver.
She needed a medical advocate. She needed me.
KnockingHeaven_ARC.indd 147
1/31/13 12:27 PM
148
katy butler
A Korean folk saying holds that after three years of caregiv-
ing, filial devotion disappears. I was lying on the couch worn
out when I got her call, looking up at the skylight. It had been
five years of back-and-forth flights, three of them in the previ-
ous eight months. Brian and I were packing for a nonrefund-
able week at a rented cabin in the mountains. I did not know
how many more years my father would last, and after that—
what then? My mother’s mother had lived to be ninety-two. My
mother might well live as long, which meant I’d be taking care of
her when I was seventy. And after that—how many years would
it be before Brian, whom I’d so far resisted marrying for reasons
I didn’t fully understand, needed my care? Who would be left
in the end to care for me? And why did most of the burden fall
on women? I called my brothers. It was their turn, I said. After
completing a weeklong acting workshop that he’d already paid
for, my brother Michael flew out. It was only his second visit
home since my father’s stroke.
Much to my relief, the doctors at Yale—New Haven decided
not to operate—a wise, “less is more” decision for which the
hospital paid a financial price. Out of $22,034 in services pro-
vided and billed, Medicare reimbursed the hospital only $6,668
under its lump-sum system—a figure that would have been far
higher, of course, if doctors had subjected my father to brain sur-
gery. All in all, the six-day hospitalization cost Medicare about
$16,891, including $8,723 for emergency, diagnostic, and doc-
tors’ services at Middlesex Memorial the first day and $1,500
for separately-billed doctors’ services at Yale—New Haven.
My mother insisted on bringing my father home as soon as she
could. He never returned to his previous “normal.” One morning,
while sitting on the couch, he asked my brother Michael why
the room was filling up with leaves. In hindsight, he’d have been
better off after his fall if my mother had not called 911 but just
washed the blood off his face and put him to bed.
KnockingHeaven_ARC.indd 148
1/31/13 12:27 PM
knocking on heaven’s door
149
*
*
*
If my parents’ seventies were golden years, their eighties were
years of lead. For the first two years after his stroke—2002 and
2003—my father and mother organized their lives around their
hope of his getting better, her determination to help him, and his
fierce motivation to regain the ability to write and speak. When
hope of true recovery ended, they marched on, my mother grow-
ing ever more lonely and exhausted, and my father accepting a
constricted life of limited but real pleasures. The fourth and fifth
poststroke years—2005 and 2006—took those pleasures from
him. His sight dimmed so much that he could no longer read
the
New York Times
. His balance became so unsteady that my
mother no longer let him walk on his own and held him up by his
belt when he walked up or down stairs. He became bowel and
bladder incontinent, and that meant the end of his water walking
at the Wesleyan pool and his lunches out twice a month with his
old colleague Richard Adelstein. His brain became so damaged
that he could not form a plan to get the bathroom on time when
he needed to but not damaged enough to keep him from being
ashamed and remorseful when Toni or my mother had to wipe
the shit from his bottom.
His life went on, thanks perhaps to his pacemaker, and he
could do nothing about it but endure. The tipping point had
come. Death would have been a blessing, and living was a curse.
As he put it to my mother one day, in his classic, understated style,
“Unfortunately, I come from long-lived people.” As Toni remem-
bered it, “He was confined to the house, and that was horrible.
He would sit in a chair with a book and just sit there. There was
nothing left for him. The only time I saw him happy was when you
visited. When you were around, he was
on the page.
He adored
you: you were Daddy’s little girl. Otherwise, it was take a nap, take
a nap, there was nothing else left. He liked to eat, and that was it.”
KnockingHeaven_ARC.indd 149
1/31/13 12:27 PM
150
katy butler
*
*
*
In California, I woke up some mornings in a fury. Why had
his doctors not let nature take its course? If the pacemaker
had never been implanted, I thought, my father might well
have been out of his misery, and so would my mother and me.
I understood very little about the device then, and I thought
that the only way to disable the pacemaker was to subject my
father to a second surgery—a path which seemed unthinkably
cruel, dangerously close to euthanasia, and, practically speak-
ing, impossible. I did not curse the mysterious ways of God, in
whom I did not believe, for keeping my father alive. I cursed
the machinery of man for disrupting the natural order, which
over millions of years of evolution had designed our hearts and
brains to fail at pretty much the same time. Where was Dr.
Rogan now, I wondered, to see what my father’s bonus years
had bought? Would he come over to my parents’ house on Pine
Street and look after my father for a single day?
When I called my brother Jonathan and vented, he joked
darkly on the phone about putting a pillow over my father’s
head. I told him about Temple Lee Stuart, a woman who lived
one town away from me in Sausalito. She’d pled guilty to man-
slaughter and was sentenced to six years in prison for smother-
ing her eighty-eight-year-old mother with a pillow in her nursing
home bed. The daughter called it a mercy killing, and main-
tained that her mother had repeatedly said she wanted to die.
Temple had been the only one of her mother’s children who
regularly visited the old lady. Temple had confessed to a brother
who lived out of town and had been arrested after he turned
her in.
On New Year’s Eve at the close of 2006, the worst, most
hopeless year so far of my father’s long life, I wrote out a prayer
in my despair and put it into my “God Box”—a coffee can onto
KnockingHeaven_ARC.indd 150
1/31/13 12:27 PM
knocking on heaven’s door
151
which I’d glued National Geographic shots of canyons, African
rock paintings, and other images of the sacred that I craved,
despite my lack of conventional religious belief. A friend in a
twelve-step program had recommended it as a technique for
letting go of what could not be fixed. “Please take care of my
mother,” I wrote. “Lead her to respite. Help me let go of trying
to control her and solve all of her problems. Help me flourish
creatively and personally whether she is happy or not. Please
help her let go, and let Jeff die.”
KnockingHeaven_ARC.indd 151
1/31/13 12:27 PM
KnockingHeaven_ARC.indd 152
1/31/13 12:27 PM
IV
Rebellion
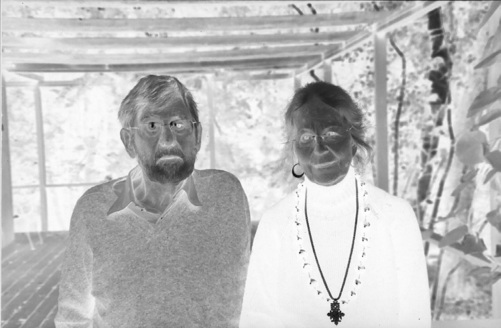
Jeffrey and Valerie Butler, Pine Street, Middletown, Connecticut, 2006.
KnockingHeaven_ARC.indd 153
1/31/13 12:27 PM
KnockingHeaven_ARC.indd 154
1/31/13 12:27 PM
The
Sorcerer’s Apprentice
In January 2007, five months after my father’s disastrous stay
at YaleNew Haven Hospital, I interviewed a woman named
Katrina Bramstedt who worked for the Cleveland Clinic. I
did not immediately understand how her work applied to my
family’s dilemmas, but soon enough I would. I was looking for
science stories to write, and she was a hospital bioethicist, a
member of a relatively new profession propelled into being by
the life-prolonging machines in the ICU. Employed by the hos-
pital, Bramstedt functioned somewhat like an informal judge,
setting out and applying the rules when families, patients, and
medical staff were at odds about whether to permit an organ
transplant, discontinue life support, insert a feeding tube, or
try a painful and possibly hopeless—and then again, possibly
lifesaving—treatment.
KnockingHeaven_ARC.indd 155
1/31/13 12:27 PM
156
katy butler
Most of her consults involved power struggles between doc-
tors and families over how to treat—or stop treating—desper-
ately ill patients in intensive care, ravaged by deadly infections
and kept alive with drugs, feeding tubes, respirators, and dialy-
sis. She had her work cut out for her. In the ICU, there was
no such thing as natural death, and few were comfortable with
the timed event that had taken its place. Half the time, doctors
wanted to keep going when families wanted to let go, and half
the time, families—especially, but not only, African-American
families—wanted to keep going when doctors wanted to quit.
Sometimes doctors ignored advance directives from patients or
even ripped them out of the chart. Sometimes a family would
balk at implanting a feeding tube in a demented relative, only to
hear a doctor say something like, “Nobody starves to death on
my watch.” Sometimes doctors complied when a long-estranged
son or daughter—commonly referred to in hospitals as “The
Nephew from Peoria”—flew in at the last minute and insisted
that everything be done, even things that doctors and other fam-
ily members thought were torturous, wasteful, and hopeless.
When fragmented families collided with a fragmented medical
system, the results could be disastrous.
An undercurrent of realistic worry ran through medical staff,
administrators, and the in-house department, usually headed
by an attorney, known as Risk Management. . In a handful of
extreme cases scattered across the country, distraught husbands
and fathers had entered ICUs with guns and disconnected a
half-dead child from a respirator or shot a comatose wife in
the head. On the other hand, if too much morphine was given,
or too little done to try to save a life, a Nephew from Peoria
might sue for negligence, or a local district attorney might
even consider charges of manslaughter. A single unnecessarily
prolonged intensive care death could cost a hospital well over
$300,000—money not recovered from Medicare, which usually
KnockingHeaven_ARC.indd 156
1/31/13 12:27 PM
knocking on heaven’s door
157
paid a lump sum based on the patient’s diagnosis, no matter
what the hospital’s costs. The families, meanwhile, were often
in shock: staggering to absorb reams of data from a rotating cast
of stranger-specialists who each zeroed in on a single organ and
did not seem to talk to each other; fearful of death; ignorant of
the limits of medicine; guilt-stricken and religiously conflicted
about ending life support; agonized by a relative’s suffering; and
hoping against hope.
In bland, untidy conference rooms edging the ICU, special-
ists asked families they’d never previously met to assent to the
removal of life support, and spouses and children pondered
questions—spiritual, legal, and medical—they’d rarely consid-
ered before tragedy hit. Did they have the right to say no to a
doctor? To force a doctor to continue treatment? Was it God’s
will to do everything possible to prolong a life, no matter how
much someone beloved was suffering? Was it suicide to refuse
medical care? Was it murder not to give it? Was it a sin? And
how were they to decide when the people they loved could no
longer speak for themselves?
Out of this ongoing moral and logistical chaos, bioethicists