Shrinks (27 page)
Authors: Jeffrey A. Lieberman
Tags: #Psychology / Mental Health, #Psychology / History, #Medical / Neuroscience
I nervously walked over and introduced myself. I asked him several questions about his study, as much to impress him with my knowledge as to deepen my understanding of his. At first he greeted me warily, but after realizing that I was a genuine admirer he warmed up and responded enthusiastically. He concluded by thanking me magisterially for my questions.
Only later did I learn that despite his fame, Kline had become something of a pariah in scientific circles. In modern parlance, he had “jumped the shark.” It should have been apparent to me at the Florida conference that his pompous behavior would be alienating to his colleagues, but as a young resident I was naïve and starstruck. I would soon learn firsthand his sins against the medical codes of conduct.
As I continued my residency at St. Vincent’s Hospital in Manhattan, I began to encounter what many psychiatrists in New York dubbed the “Kline experience.” Patients of Dr. Kline began to drift into the emergency room and the outpatient clinic, and as new admissions to the psychiatric inpatient unit. All were victims of Kline’s risky and sometimes heedless practice. They suffered from severe adverse reactions caused by elaborate cocktails of psychotropic medications—or from the effects of their abrupt withdrawal. Whereas most psychiatrists treated depression, bipolar disorder, schizophrenia, or anxiety disorders by prescribing one or two medications, possibly three on a rare occasion, Dr. Kline frequently prescribed extravagant combinations of five or more medications in their most potent forms, often at high doses. It got to the point where I was able to guess whether a patient was one of Kline’s simply by glancing at the list of medications on his chart. No one else had the confidence—or recklessness—to prescribe such witches’ brews of mind-altering cocktails.
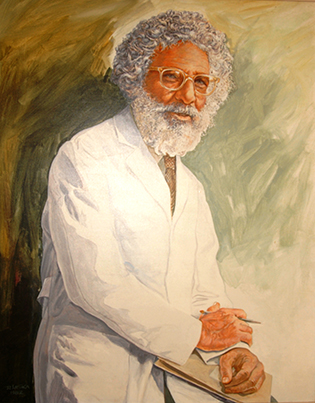
Nathan Kline (1916–83), a flamboyant pioneer of psychopharmacology. (Portrait of Dr. Kline by David Laska, courtesy of Dr. Eugene Laska and the Nathan S. Kline Institute for Psychiatric Research, Orangeburg, NY; photograph courtesy of Koon-Sea Hui, MPhil, PhD)
In the end, it was not the death of a patient or a massive malpractice suit that prompted Kline’s downfall, though that was surely a possibility. It was the very study that had inspired me to timidly seek an audience with him in Florida. Kline had failed to submit the protocol for his study to an Institutional Review Board for approval, an ethical and legal requirement when conducting medical research on human subjects. Not only that, he hadn’t bothered to get the proper informed consent from the patients to whom he was administering experimental psychoactive compounds. Apparently, in his eagerness to achieve another stunning scientific success (and perhaps win a Nobel), he had rushed to be the very first researcher to publish on a potential new class of psychopharmaceutical.
The FDA investigated Kline, and in 1982 he was compelled to sign a federal consent decree swearing to never conduct research on drugs again. Psychoactive drugs had launched Kline’s career—and they ended it in ignominy. A year later, he died on an operating table from complications arising from an aortic aneurysm.
Despite Kline’s excesses, the advent of psychopharmacology had irrevocably changed the field of psychiatry for the better. Those suffering from severe mental illness now could hope for relief and genuine recovery. But it also created tensions in a field struggling to redefine itself. This quandary was not lost on the media, which laid bare the emerging ideological fault lines. In 1955, in the wake of chlorpromazine’s redesign of the mental health landscape,
Time
magazine reported, “The ivory-tower critics (mainly psychoanalysts) argue that the red-brick pragmatists—state hospitals—are not getting to the patients’ ‘underlying psychopathology’ and so there can be no cure. These doctors want to know whether he withdrew from the world because of unconscious conflict over incestuous urges or stealing from his brother’s piggy bank at the age of five. In the world of red-bricks, this is like arguing about the number of angels on the point of a pin.”
But before the psychopharmacologists could permanently tip the balance away from the ivory-tower psychoanalysts, one final revolution was still necessary.

If there is one central intellectual reality at the end of the twentieth century, it is that the biological approach to psychiatry—treating mental illness as a genetically influenced disorder of brain chemistry—has been a smashing success. Freud’s ideas, which dominated the history of psychiatry for much of the past century, are now vanishing like the last snows of winter.
—E
DWARD
S
HORTER
Out of the Wilderness: The Brain Revolution
Here is this three-pound mass of jelly you can hold in the palm of your hand, and it can contemplate the vastness of interstellar space. It can contemplate the meaning of infinity and it can contemplate itself contemplating on the meaning of infinity.
—V
ILAYANUR
R
AMACHANDRAN
Every pusillanimous creature that crawls on the earth or slinks through slimy seas has a brain!
—
T
HE
W
IZARD OF
O
Z
If I Only Had a Brain
In
The Wizard of Oz
, the Scarecrow yearns for a brain. To his surprise, the Wizard informs him that he already possesses one—he just doesn’t know it. For most of the twentieth century, the same might have been said about psychiatry—it was brainless. Though ostensibly a medical specialty devoted to abnormalities of thought and emotion, psychiatry did not turn its attention to the
organ
of thought and emotion until the 1980s.
Psychiatrists were not alone in ignoring the brain—the level of interest in the pinkish stuffing inside our heads has long been woefully disproportionate to its importance, especially when compared to its main rival for anatomical preeminence: the heart. When we marry or fall in love, we give our
heart
to another, but never our brain. When someone leaves us we feel
heartbroken
, not
brainbroken
. Generous people are said to have
big hearts
or be
good-hearted
or have
hearts of gold
rather than
brains of gold
. Even the Bible invests the heart with psychic properties: “And you shall love the Lord your God with all your heart.”
But the heart is nothing more than a glorified pump. Its sole function is to contract and expand, over and over, two billion times over the average lifespan, pushing blood through the body. In contrast, the human brain is an unfathomable supercomputer that exceeds every other organ in complexity by many orders of magnitude. Starting as an unimaginably tiny neural tube forming three weeks after conception, the brain grows at an astonishingly rapid pace to become a three-pound corrugated doughlike lump—comprising a hundred billion neurons communicating through thirty trillion connections—that somehow regulates our heart rate, body temperature, and appetite while simultaneously driving us to sing melodies, sculpt statues, code software… and pen lengthy treatises about itself. Comparing the heart to the brain is like comparing a child’s dollhouse to New York City.
One thing that has always confounded any researcher wishing to scrutinize the brain is the fact that this arcane supermachine is encased within an impenetrable vessel: the skull. Until very recently, the only way to actually
examine
a thinking, feeling brain was through extremely invasive procedures or by carving up a lifeless brain at autopsy. It’s not very surprising that the first science-tinged theory of the brain was founded on a rather ingenious (if completely misguided) method of circumventing the need to directly access the brain:
phrenology
.
Developed by the German physician Franz Joseph Gall in 1809, phrenology took as its starting point the assumption that different parts of the brain controlled specific functions. One region controlled hunger, another controlled lust, another anger. As neuroscientists would later confirm, this assumption turned out to be largely correct: specific mental functions are indeed localized in specific brain regions. Gall’s next two hypotheses were not so lucky, though. He believed that if a person exhibited disproportionate activity issuing from a particular mental function—excessive lust, for instance—then (1) the part of his brain that governed lust would be enlarged, and (2) the skull above this enlarged part of his brain would also be enlarged. Thus, Gall claimed it was possible to discern a person’s true psychological constitution by measuring the relative size of the various bumps and indentations on his head. You might say that phrenology was the world’s first crude attempt at brain mapping.
Gall diligently appraised the skull geometries of prisoners, hospital patients, and asylum lunatics, and reported many sensational “findings.” The heads of the stark raving mad featured a depression toward the back of their skull, which Gall interpreted as indicating a diminishment of their faculty of self-control. Young thieves possessed bumps just above their ears. All of these purported correlations between skull geometries and behavior turned out to be completely groundless. We now know there is no connection between a person’s personality and the shape of his head.
Unable to provide any useful predictions about human behavior, phrenology had completely fallen out of favor by the middle of the nineteenth century, about the same time that Wilhelm Griesinger declared that mental illnesses were “illnesses of the nerves and brain.”
A century later, in the late 1940s and ’50s, the first cohort of brain-focused psychiatrists began to emerge in American psychiatry. Though they were far outnumbered by the Freudians, members of organizations like the Society of Biological Psychiatry revived the brain-focused studies of their German forebears. But they did not limit themselves to the examination of postmortem specimens; they also trolled for clues in the bodily fluids of living patients—the blood, cerebral spinal fluid, and urine. The new generation of biological psychiatrists believed that somewhere in this organic soup they would find their Holy Grail: a biological marker for mental illness.
Just as John Cade believed that mania was produced by a metabolic toxin, the biological psychiatrists hypothesized that mental illness might be caused by some pathogenic organic compound aberrantly produced by the body—a compound presumably detectable through laboratory tests. The inspiration for this hypothesis was a metabolic disorder known as phenylketonuria (PKU), a condition caused by a genetic mutation that prevents the liver from metabolizing phenylalanine, an essential amino acid. The faulty metabolism in individuals with PKU produces an accumulation of a substance known as
phenylketone
. Too much phenylketone interferes with the brain’s development and leads to intellectual disability and behavioral problems. Thus, phenylketone serves as a biomarker for PKU: If physicians detect the compound in a patient’s blood or urine, it indicates he probably has the disorder, since people without this condition have extremely low levels of phenylketone.