i bc27f85be50b71b1 (62 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown
\1USCUlOSKHFTAL SYSTEM
197
Figure 3-15. Umc()mpartmental knee arthroplasty of the Tight medial
compartment.
an increased ROM is obtained because of more normal kinematics of
the knee joint. Revision from a unicompartmental to a tricompartmental knee arthroplasry is ofren warramed ar a larer rime because of continued degeneration; however, newer unicompartmental prosthetic designs may show improved results.4s Associated valgus deformiries may also be correcred by a ribial osreoromy and release of sofr (issue during rhe partial knee replacement.
The tricompartmelltal or total kllee arthroplasty (TKA) is rhe
replacemenr of rhe femoral condyles, rhe ribial articularing surface, and
rhe dorsal surface of rhe parella. This rype of knee arthroplasry involves
replacing rhe medial and lateral comparrmenrs of the joinr, as well as
resurfacing the patellofemoral articulation with prosthetic components
( Figure 3-16A). These componenrs are made of marerials similar ro
rhose of rhe THA. The femoral condyles are replaced wirh a meral
bearing surface rhar articulares wirh a polyerhylene rray implanred on
rhe proximal ribia. The dorsal aspect of rhe parella is ofren resurfaced if
excessive erosion of the cartilage has occurred; however, some surgeons
refrain from rhe parellar implanr if rhe arricular cartilage of the patella
seems reasonably intact, as shown in Figure 3-16B.46


198 ACUTE CARE HANDBOOK FOR PHYSICAL TI IERAPISTS
A
B
Figure 3� 16. A. Anterior view of a right total knee arthroplasty. B. Lateral
view of a right total knee arthroplast),.
The methods of fixation in TKA are similar to those of hip replacemenr. Cementing techniques can be used to fix the components, or the prosthetic design can allow for either porous ingrowth or press-fir. A
press�fit prosthesis has surface modifications or grooves and bioactive
hydroxyapatite to provide macrointerlock with the bone.'o Many sur-

MUSCUlOSKELI;�rAL SYSTEM
199
geons tend to use a hybrid technique by using a cemented tibial component with porous coated femoral and patellar prostheses. Partial weight bearing or weight bearing as tolerated often is allowed after TKA and is
encouraged to promote use of the limb and promote bone remodeling.46
Patients who undergo either type of knee arthroplasty may have
associated preoperative soft tissue contractures. A lateral retinacular
release can be performed to centralize patellar tracking. If performed,
there may be an increased risk of patellar subluxation with flexion.
Special procedures that are performed in either type of knee arthroplasty should be taken into consideration by the physical therapist, because the surgeon may impose restrictions to ROM and weight
bearing. Any additional procedure may prolong healing time secondary to increased edema and pain, which limits the patient's functional mobility and wlerance w exercise.
General medical complications after TKA are similar to those
described with THA. Table 3-7 lists common complications specific
to TKA.
Physical Therapy Intervention after Knee Arthroplasty
Physical therapy intervention after knee arthroplasty is focused on
increasing functional independence. The patients muSt also perform
ROM and strengthening exercises and be educated in positioning
techniques to help reduce swelling. Restrictions on weight bearing
and precautions are also taught to the patient.
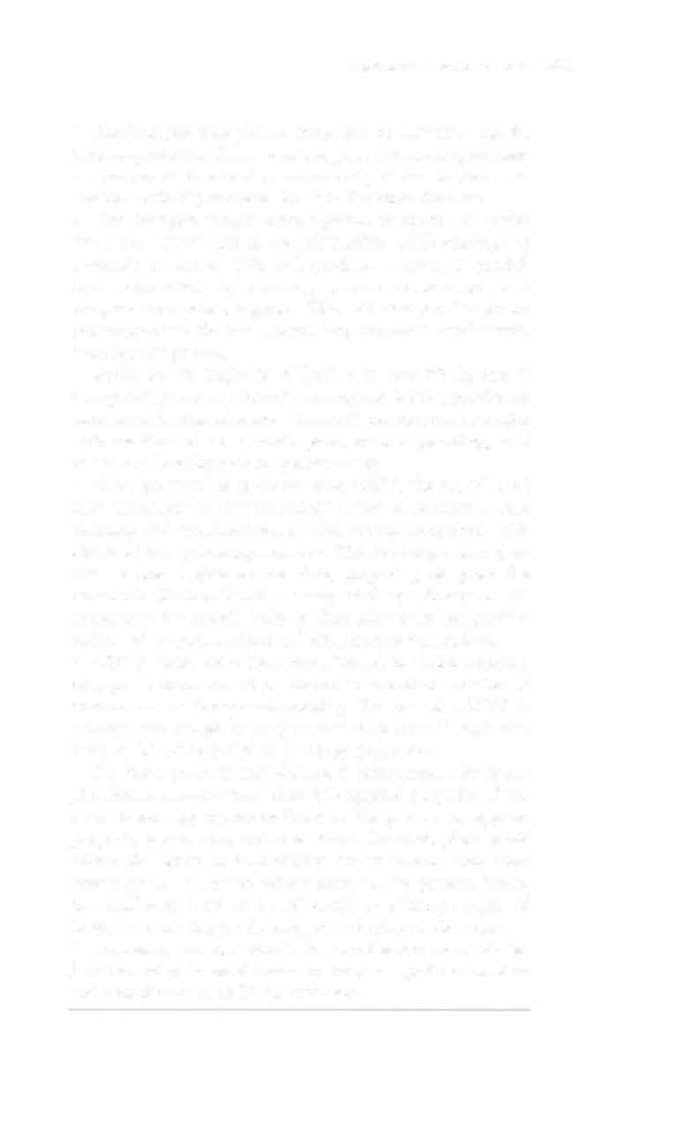
Table 3-7. Complications after Total Knee Anhroplasty
Thrombosis and rhromboembolism
Poor wound healing
Infecrion
Joim insrability
Fracrures
Patellar tendon rupture
Parellofemoral instability, component failure, or loosening
Peroneal nerve injury
Component loosening or breakage
Wear and deformation
Source: Adaprcd from JL Guyron. Anhroplasry of Ankle and Knec. In ST Canale ( cd),
Campbell's Oper:ltive Orrhop:lcdics, Vol. I (9th cd). $(. LOllis: Mosby, 1998.
200
AClITE CARE HANDBOOK FOR PHYSICAL THERAPIST'S
• Evaluation and treatment of functional mobility to promote
independence should begin immediately postoperatively. Bed
mobility, transfer training, and gait training on level surfaces and
stairs with appropriate assistive devices should be instructed to the
patient to maximize functional outcomes and safety.
• Strengthening exercises may begin immediately postoperatively,
emphasizing quadriceps exercises. Quadriceps retraining may be
accomplished with overflow from the uninvolved limb or distal
limb. Active-assisted quadriceps exercises should be performed to
increase stability around the operated knee. The patient should be
encouraged to perform exercises independently, within the limits of
comfort.
• Knee immobilizers are often prescribed to protect the knee from
twisting and buckling secondary to decreased quadriceps strength.
With a lateral release, there may be increased pain and edema that
may hinder quadriceps functioning; therefore, a knee immobilizer
or brace may be required for a longer period of time.
•
ROM exercises should begin immediately after TKA. ROM
must be gained early in the rehabilitation of a TKA and is accomplished by passive or active-assisted exercises. If available, a continuous passive motion (CPM) machine may be used immediately postoperatively. The limitations to ROM are often attributed to
pain, swelling, muscle guarding, and apprehension, all of which
can be addressed through physical therapy interventions and
patient education.
• Positioning and edema control should be initiated immediately
to help reduce pain and increase ROM. The patient should be educated to elevate the operated extremity with pillows or towel rolls under the calf to promote edema reduction and promote knee
extension. Ice should be applied after exercise or whenever needed
for patient comfort.
Clinical Tip
•
Educate the patient to elevate the operated limb without putting pillows or towel rolls under the knee. This
type of positioning keeps the knee flexed and will increase
the risk of flexion contractu res and edema.
MUSCULOSKE.LETAL SYSTE.M
201
• The therapist may place a towel roll or blanket along the
lareral aspect of the femur, near the greater trochantet, to maintain the operated extremity in a neutral position. Any external rotation at the hip can result in slight flexion at the knee.
• The therapist should place a pillow or towel roll under
the knee in the degree of available ROM while performing
isometric exercises. This will produce a stronger quadriceps contraction by reducing passive stretch on joint
receptors and pain receptors. This will also provide posterior suppOrt to the knee, providing increased tactile feedback for the patient.
• ROM for the majority of TKA is at least 90 degrees in
rhe operating room. Consult the surgeon for the maximum
amount of flexion obtained. This will provide the therapist
with an idea of how much pain, muscle guarding, and
edema are limiting patient performance.
• When performing active-assistive ROM, the use of hold!
relax techniques to the hamstrings assists to decrease muscle
guarding and increases knee flexion through reciprocal inhibition of the quadriceps muscle. This technique also provides a dorsal glide to the tibia, preparing the posterior capsule for flexion. Gentle massage of the quadriceps mechanism over the muscle belly or throughout the peri patellar region will improve ROM and reduce muscle guarding.