i bc27f85be50b71b1 (51 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown



MUSCULOSKELETAL SYSTEM
165
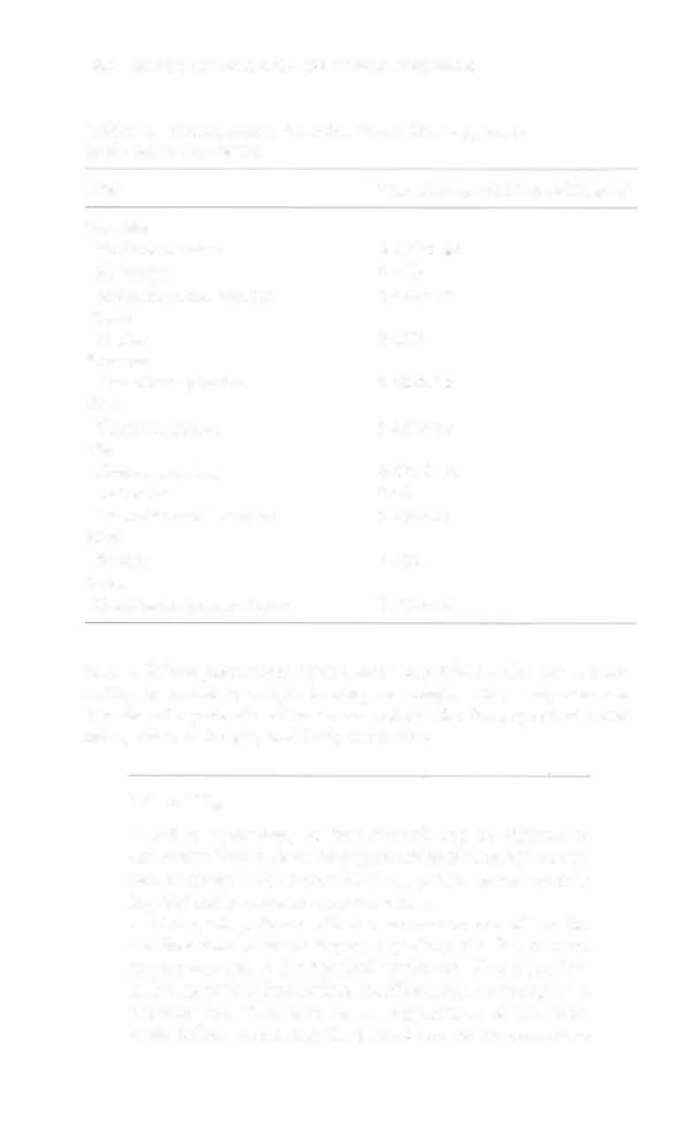
Table 3-2. Lower-Quarter Screen
Nervc
Deep Tendon
Root
Myorome
Dermarome
Reflex
L 1
Hip flexion
Antero-superior thigh just
None
below the inguinal ligament
L2
Hip flexion
Anterior medial thigh 2.5 in.
None
below the anterior superior
iliac spine
L3
Knee extension
Middle third of anterior thigh
None
with L4
L4
Knee extension
Pacclla and medial malleolus
Patellar
with L3 and LS
tendon
L4,S
Ankle
None
dorsiflexion
LS
Great toe
Fibular head and dorsum of
Posterior
extension
foot
tibialis
51
Ankle plantar
Lateral malleolus and plantar
Achilles ten-
flexion
surface of foot
don
Sources: Adapted from ML Palmer, ME Epler (cds). Clinical Assessmem Procedures
in Physical Therapy. Philadelphia: Lippincotf, 1990;33; and data from S HoppenfeId. Physical Examination of the Spine and Extremities. Norwalk, CT: Appleron & Lange, 1976.
in terms of qualiry or movement through an ROM (e.g.,
active hip flexion is one-third range in supine).
• Sen ory testing is especially important over moderately
or severely edematous areas, especially the distal extremities. The patient may not be aware of subtle changes in sensation.
•
Girth measurements may be taken if edema of an
extremity subjectively appears to increase.
Functional Mobility and Safety
Functional mobility, including bed mobility, transfers, and ambulation on level surfaces and stairs, should be evaluated according to activity level, medical-surgical stabiliry, and prior functional level.
Safety is a key component of function. Evaluate the patient'S willing-
166
AClffE CARE HANDBOOK FOR PHYSICAL THERAPISTS
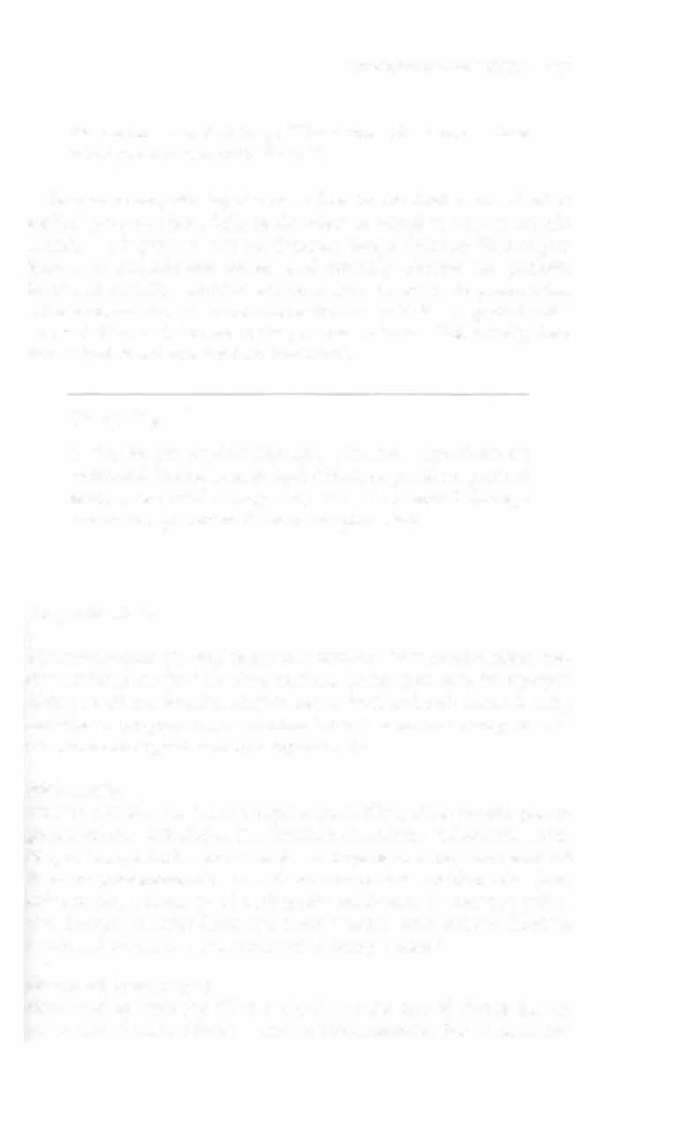
Table 3-3. Normal Range of Morion Values Mosr Applicable
in the Acute Care Setting
Joint
Normal Range of Morion (Degrees)
Shoulder
Flexion/extension
0-18010-60
Abduction
0-180
Internal/external rotation
0-7010-90
Elbow
Flexion
0-150
Forearm
Pronation/supination
0-8010-80
Wrist
Flexionlextension
0-8010-70
Hip
Flexion/extension
0-120/0-30
Abducrion
0-45
Internal/external rotation
0-4510-45
Knee
Flexion
0-135
Ankle
Dorsiflexion/plantar flexion
0-2010-45
ness to follow precautions with consistency. Observe for the patient'S
ability to maintain weight bearing or comply with equipment use.
Monitor the patient'S self-awareness of risk for falls, speed of movement, onset of fatigue, and body mechanics.
Clinical Tip
•
Safety awareness, or lack thereof, can be difficult to
document. Try to describe a patient'S level of safety awareness as objectively as possible (e.g., patient leaned on roiling tray table, unaware it could move).
• Nearly all patients will fear movement out of bed for
the first time to some degree, especially if a fall or traumatic event led to the hospital admission. This is particularly true with elders. Before mobilization, use strategies to decrease fear. This includes an explanation of the treatment before mobilizing the patient and of the sensations


MUSCULOSKELETAL SYSTEM
167
the patient may feel (e.g., "Your foot will throb a little
when you lower it to the floor.").
Because orthopedic injuries can often be the final result of other
medical problems (e.g., balance disorders or visual or sensory impairments), it is important that the therapist take a thorough history, perform a musculoskeletal screen, and critically observe the patient's functional mobility. Medical problems may be subtle in presentation
but may dramatically influence the patient's capabilities, especially with
new variables, such as pain or the presence of a cast. Collectively, these
factors lead to a decreased functional level.
Clinical Tip
It may be the physical therapist who first appreciates an
additional fracture, neurologic deficit, or pertinent piece of
medical or social history. Any and all abnormal findings
should be reported to the nurse or physician.
Diagnostic Tests
The mOSt commonly used diagnostic tests for the musculoskeletal system are listed in the following sections. These tests may be repeated during or after a hospital stay to assess bone and soft tissue healing
and disease progression, or whether there is a sudden change in vascular or neurological status postoperatively.
Radiography
More commonly known as x-rays or plain films, radiographic photographs are the mainstay in the detection of fracture, dislocation, bone loss, or foreign bodies or air in tissue. Sequential x-rays are standard
intra- or postoperatively to evaluate component position with joint
arthroplasty, placement of orthopedic hardware, or fracture reduction. X-rays may also detect soft tissue injuries, such as joint effusion, tendon calcification, or the presence of ectopic bone.'
Computed Tomography
Computed tomography (CT) is the diagnostic test of choice for the
evaluation of conical bone in certain circumstances. For fracture and
168 ACUTE CARE HANDBOOK FOR PHYSICAL THERAPISTS
dislocations, CT can provide three-dimensional views for the spatial
relationship of fracture fragments or to further evaluate fracture in