i bc27f85be50b71b1 (52 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown
anatomically complex joints, such as the pelvis, sacrum, spine, or
shoulder.' CT is commonly used to define and localize spinal stenosis,
disc protrusion or herniation, nerve entrapment, bone tumor, and
osseous or articular bone infection or abscess.4
Magnetic Resonance Imaging
Magnetic resonance imaging (MRJ) is superior to x-ray or CT for the
evaluation of soft tissue. MRI detects partial or complete tendon, ligament, or meniscal tears. MRI has also been used to (1) detect patellar tracking abnormalities, rOtator cuff rcars, and arthritis; (2) detect and
localize soft tissue masses, such as hematoma, cyst, abscess, or lipoma;
and (3) evaluate bone marrow. Finally, the high resolution of MRJ reveals
stress fractures and bone bruises that could be unobserved on x-ray.'
Bone Scan
A bone scan is the radiograpllic picture of the uptake in bone of a radio
onuclide tracer. Scans of a portion of or the whole body may be taken
at the instant rhe tracer is injected or 5-1 0 minutes or 2-4 hours postinjection. Bone scan reAects the metabolic sratus of the skeleton at the time of the scan and is extremely helpful in detecting metabolic abnor·
malities of bone before the appearance of structural changes on x-ray.s
It is therefore used to detect skeletal metastases, especially in the base of
the skull, sternum, scapula, and anterior ribs.s Other uses of bone scan
include the diagnosis of stress fractures and other nondisplaced fractures, early osteomyelitis, inAammatory or degenerative arthritis, avascular necrosis (AVN), and myositis ossificans.
Arthrography
An arthrogram is a radiograph of a joint with air or dye cOntrast. Performed primarily on the knee, shoulder, and hip, arthrography allows examination for internal joint derangements or soft tissue disruption.
Arrhrograms may diagnose meniscal and cruciate ligament tears or
articular cartilage abnormalities of the knee, adhesive capsulitis or
rotator cuff tears of the shoulder, and arthritis or intra-articular neoplasm of the hip.'
Myelography
A myelogram is a radiograph or CT of the spinal cord, nerve root,
and dura mater with dye contrast. A myelogram can demonstrate spi-



MUSCULOSKEU-rAL SYSTEM 169
nal stenosis, cord compression, intervertebral disc rupture, or nerve
root injury.1
Clinical Tip
• X-rays may be ordered after any new event, such as an
in-hospital fall, abnormal angulation of an extremity, possible loss of fixation or reduction, or for a dramatic
inctease in pain. Regatdless of the situation, defer physical
therapy intervention until results are reported or the situation is managed.
• Physical therapy intervention is typically deferted for
the patient POSt myelography secondary to specific postprocedure positioning and bed test restrictions. (Refer to Myelography in Chaptet 4.)
• As with any test that includes contrast media, contrastrelated reactions post arthrogram or myelogram may
occur. Check with the nutse or physician befote physical
therapy intervention.
Fracture Management
Types of Fracture
The analysis and classification of fracture reveal the amount of energy
impacted on bone and the potential for secondary injury, and direct
fracture management. Fractures can be described according to the
followings:
1. The maintenance of skin integrity:
a. A closed fractllre is a bony fracture withour disruption of the skin.
b. An opel! fractllre is a bony fracture with open laceration of the skin or protrusion of the bone through the
skin.
2. The site of the fracture:

170 ACUTE CARE HANDBOOK FOR PHYSICAL THERAPISTS
a. At the proximal third, distal third, or at the shaft of
long bones.
b. An intra-articular fracture involves the articular surface. Intra-articular fractures are furrher described as linear, comminuted, impacted, or with bone loss. An extraarticular fracture does not involve the arricular surface.
c.
An epiphyseal {racture involves the growth plate.
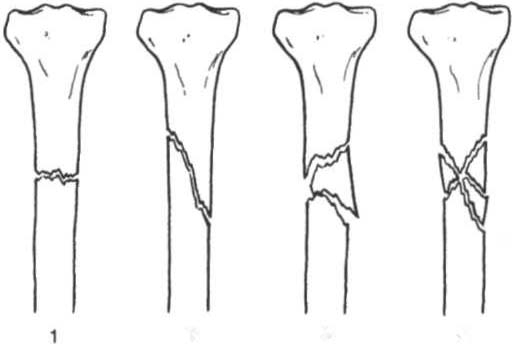
3. The configuration of the fracture (Figure 3-1):
a.
A linear fracture can be transverse (fracture is perpendicular to the long axis of the bone), oblique (fracture is on a diagonal to the long axis of the bone), or spiral
(fracture is similar to oblique with a greater surface area
of shaft involvement secondary to a circular pattern).
b. A comminuted {racture has two or more fragments.
A burterfly (wedge-shaped) fragment may or may not be
present.
e.
A segmental fractllre has two or more fracture lines
at different levels of the bone.
2
3
4
Fig'ure 3-1. Orientation of a fracture pattern. (1 = transverse; 2 = oblique; 3 =
segmental; 4 = comminuted.) (With permission from A Unwin, K Jones reds/.
Emergency Orthopaedics and Trauma. Boston: Butterworth-Heinemann,
1995;22.)
MUSCULOSKELETAL SYSTEM 171
4.
The extent of the fracture:
a. An incomplete fracture, in which one portion of the
cortex is interrupted.
b. A complete (ractllre, in which all cortices of bone are
interrupted.
5. The relative position of the fragments:
a. A flofldisplaced (rac/llre is characterized by anatomic
alignment of fracture fragments.
b. A displaced fracture is characterized by abnormal
anatomic alignmem of fracture fragments.
Cliflical Goal o( Frac/llre Management
The goal of fracrure management is bony union of the fracture without further bone or soft tissue damage that enables early testoration of maximal function.9 Early restoration of function minimizes cardiopulmonary compromise, muscle atrophy, and the loss of functional ROM. It also minimizes impairments associated with limited skeletal weight bearing (e.g., osteoporosis).
Fractures are managed either nonoperatively or operatively on an
elective, urgent, or emergent basis depending on the location and type
of fracture, presence of secondary injuries, and hemodynamic stabiliry. Elective or floflllrgellt management (days to weeks) applies to stable fractures with an intact neurovascular system or fracture previously managed with conservative measures that have failed.
Urgeflt management (24-72 hours) applies ro closed, unstable fractures, dislocations, or long bone stabilization with an intact neurovascular system. Emergent management applies to open fractures, fractures/dislocations with an impaired neurovascular system or compartment syndrome, and spinal injuries with deteriorating neurologic deficits.'
Fracture redllctiofl is the process of aligning and approximating
fracture fragments. Reduction may be achieved by either closed or
open methods. Closed redllction is noninvasive and is achieved by
manual manipulation or traction. Open reduction internal fixation
(ORIF) techniques require surgery and fixation devices (Figure 3-2),
commonly referred to as hardtl/are. ORIF is the treatment of choice
